Necessity is the mother of invention. It’s a phrase that many of us have likely heard before, and it’s one that, in many ways, encapsulates how agile the world has had to be in navigating the curveball that was the year 2020.
To combat the various challenges that have arrived with the COVID-19 pandemic, a range of Australian government health initiatives have been mobilised to adapt to the changing healthcare landscape.
Electronic Prescribing
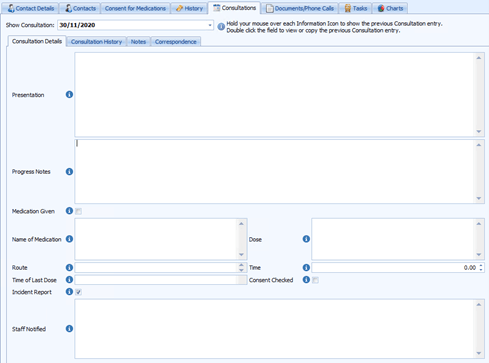
Arguably the most impactful of 2020’s Australian government health initiatives was the fast-tracking of the ePrescribing rollout. With Practices closing to walk-in patients and reverting almost entirely to remote and telehealth consultations, Electronic Prescribing was the next logical step in minimising risk to both doctors and patients.
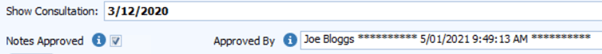
To assist with the introduction of ePrescribing in the Bp Premier Jade SP3 update, we produced a range of content helping Practices to get started with ePrescribing, our training team produced an Electronic Prescribing Masterclass, and we were proud to announce that Australia’s first ePrescription was processed through Bp Premier in May 2020.
While Electronic Prescribing has been an invaluable tool during the COVID-19 pandemic, the convenience it offers both doctors and patients is a benefit that will remain a constant well into the future.
Secure Messaging
A core part of healthcare in Australia today is the ongoing communication between healthcare providers. As is the nature of discussing medical issues, many of the communications are sensitive in nature, and are often transmitted over unsecure channels, or channels that experience incompatibilities – leading to the potential of communication breakdown, poor outcomes and an inefficient transfer of information.
The national Australian government health initiative on Secure Messaging was agreed upon in 2019 and began work in 2020 in an effort to improve the encrypted electronic exchange of patient healthcare information between healthcare providers. Typical use cases included discharge summaries, referrals and requests and the receipt of results.
Bp Software’s Commercial and Customer Enablement Manager Monica Reed wrote an article on the Secure Messaging initiative, outlining the importance of the functionality, how Best Practice Software got involved, and when Practices can expect Enhanced Secure Messaging to be more widely available.
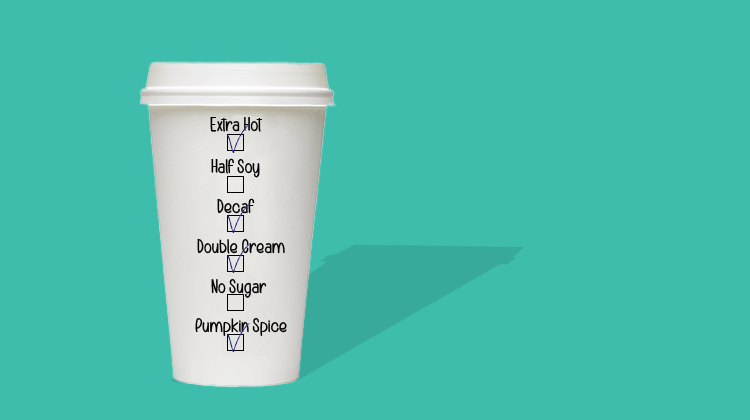
Active Ingredient Prescribing
From February 2021, prescribing medication by its active ingredient will be a mandatory requirement. This was announced alongside the government’s 2018-2019 Electronic Prescribing budget, and means Practices will need to be on the latest software version to comply, Bp Premier Saffron and Bp VIP.net Ruby SP3.
The regulation mandates the inclusion of active ingredients on all PBS and RPBS prescriptions, with exceptions for handwritten prescriptions, paper-based medication charts in residential aged care settings. medicines with four or more active ingredients and non-medicinal items which don’t have active ingredients (e.g. dressings, nutritional products). Brand names will be able to be included in the prescription if deemed clinically necessary by the prescriber, but the active ingredient will still need to be listed first as per regulations.
To help prepare our customers for this change, we produced an introductory article, outlining what Active Ingredient Prescribing would mean for your Practice, as well as videos explaining the process and impact of the initiative on both patients and practitioners – helping to bring everyone up to speed before the regulations take effect in early 2021.
Real-Time Prescription Monitoring
Though technically introduced late in 2019, the National Real Time Prescription Monitoring (RTPM) initiative has seen significant progress in 2020.
The misuse of controlled substances and medication is an area of growing concern. The RTPM initiative is designed to help reduce the misuse of controlled substances, while ensuring that patients who genuinely need these medications can still get them. The RTPM initiative consists of a National Data Exchange (NDE), and regulatory systems managed by each individual state or territory.
States are now working to integrate their regulatory systems with the database – as we’ve seen successfully occur with Victoria’s SafeScripts platform, and the soon to be delivered ScriptCheckSA in South Australia.
Read more about the Real Time Prescription Monitoring initiative here.
National Cancer Screening Register
The last, but certainly not least among 2020’s important initiatives was the National Cancer Screening Register (NCSR), and this integration is available in Bp Premier with our latest Saffron release.
The NCSR is a Department of Health initiative developed to encourage and support bowel cancer and cervical cancer screening. The register has been developed by Telstra Health in partnership with state and territory governments. We’ve partnered with Telstra Health and government departments to integrate the NCSR with Bp Premier to enable simple electronic capture of cancer related health information.
The NCSR provides a range of significant benefits to patients – such as screening reminders and having their doctor make better informed decision with access to their screening history, but it benefits practitioners as well through the ability to order screening test kits, receiving reminders for patients who are overdue for a screening or follow-up, and manage their patients’ program participation.
All of this is now accessible through Bp Premier’s Saffron release, and you can read an article on the National Cancer Screening Register initiative here.
Australian Government Health Initiatives in 2021
Electronic Prescription Token Solution to Integrate with Medisecure
In supporting 2020’s ePrescribing rollout, and the initial introduction of an electronic prescribing token solution integrated with the eRx prescription exchange service, Bp Software will introduce an electronic prescribing token solution integrated with the Medisecure prescription exchange service in Saffron SP1.
We’ve listened to the feedback and understood that a choice of prescription exchange is important to our GP users, so we are working together with Medisecure to deliver this in our next release.
Supporting the Active Script List
In 2021 we’ll be working with the relevant government bodies to extend Bp Premier’s Electronic Prescribing functionality to support the Active Script List. Currently, when a patient seeks to fill a prescription electronically, they do so via a token on their electronic device. A token that is lost, misplaced or accidentally deleted needs to be resent to the patient by the Practice.
Under the Active Script List initiative, pharmacists will be able to verify a patient’s identity and view their valid electronic prescriptions, then safely dispense the necessary medications.
The primary goal of the Active Script List is to overcome the issue of lost tokens, and assist medication management and adherence, especially for patients who are on a schedule of multiple medications.
Medicare Web Services
The Medicare Client Adaptor is how providers currently connect to Medicare Online Claiming, however the technology is quickly becoming dated and providers are being encouraged to transition to the new method of connection, called Web Services. From the 13th of March in 2022, the Medicare Client Adaptor will be retired and no longer accessible.
Currently, Bp Premier and Bp VIP.net connect to Services Australia using the Medicare Client Adaptor. However, due to the eventual transition over to Web Services, there is significant work being undertaken to update Bp Premier and Bp VIP.net to utilise this newer method of authentication and connection.
You can read more about Medicare Web Services here.
COVID-19 Vaccine Reporting Initiatives
Currently in Australia, the recording of vaccinations is encouraged, but not mandatory. A bill currently moving through Australian Parliament will compel GPs and other vaccine providers to report all newly administered vaccines to the Australian Immunisation Register. The aim of the bill is to support the rollout of the COVID-19 vaccine, and the ongoing administration of the National Immunisation Program.
In preparation of the national rollout of the COVID-19 vaccine, Bp Premier’s latest Saffron release provides the functionality to record a patient’s vaccine serial number.
Bp Software is committed and actively participating in government and industry information sessions to ensure that, as we learn more about the mandatory reporting requirements and anticipated upload of vaccine data to the Australian Immunisation Register, we can ensure that our products will comply with user needs.
2020 presented the world, and the healthcare industry in particular, with many unique challenges. While many of the Australian government health initiatives outlined above already had wheels in motion, the fast tracking and prioritising of their rollouts have helped the healthcare industry to remain adaptive to a rapidly shifting landscape.
Important initiatives continue to be the focus in 2021, and will no doubt help to strengthen the Australian healthcare industry – offering innumerable benefits for providers, practitioners and patients alike.