We are excited to announce the official release of our Online Booking Management Solution, Best Health Booking.
Best Health Booking integrates with Bp Premier to provide a hassle-free booking solution for practice managers and practice owners. It also provides convenience to patients and streamlines administrative tasks, all while being easy to navigate and configure.
Best Health Booking has been through rigorous Beta Testing and was designed in partnership with Bp Premier customers.
“Listening to our customer’s feedback provided clear direction for which features would be most beneficial to their clinics when it came to an Online Appointment Booking Solution. Based on beta testing and ongoing feedback received, we are sure Bp Premier customers will be thrilled with Best Health Booking overall, but especially the seamless integration, simple setup and maintenance and the patient convenience it offers,” Ms Danielle Bancroft, our Chief Product Officer, explained.
To determine whether Best Health Booking is right for your clinic, we encourage you to visit our website.
How Will Best Health Booking Help Your Practice?
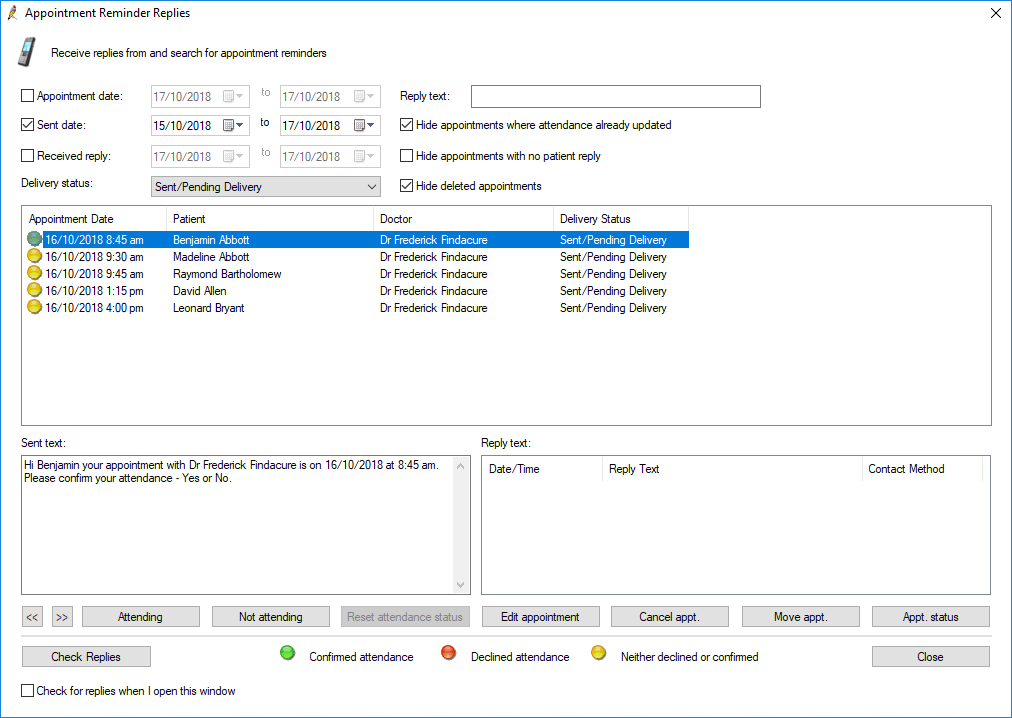
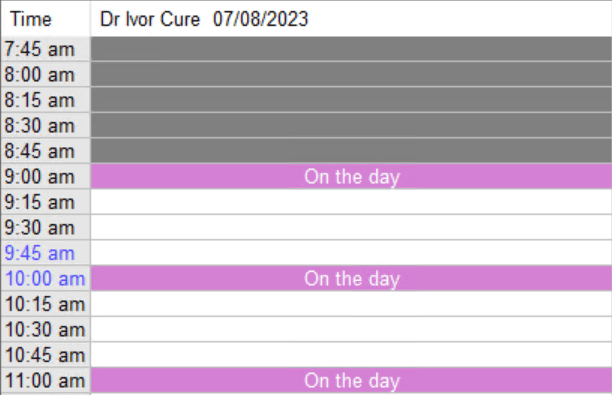
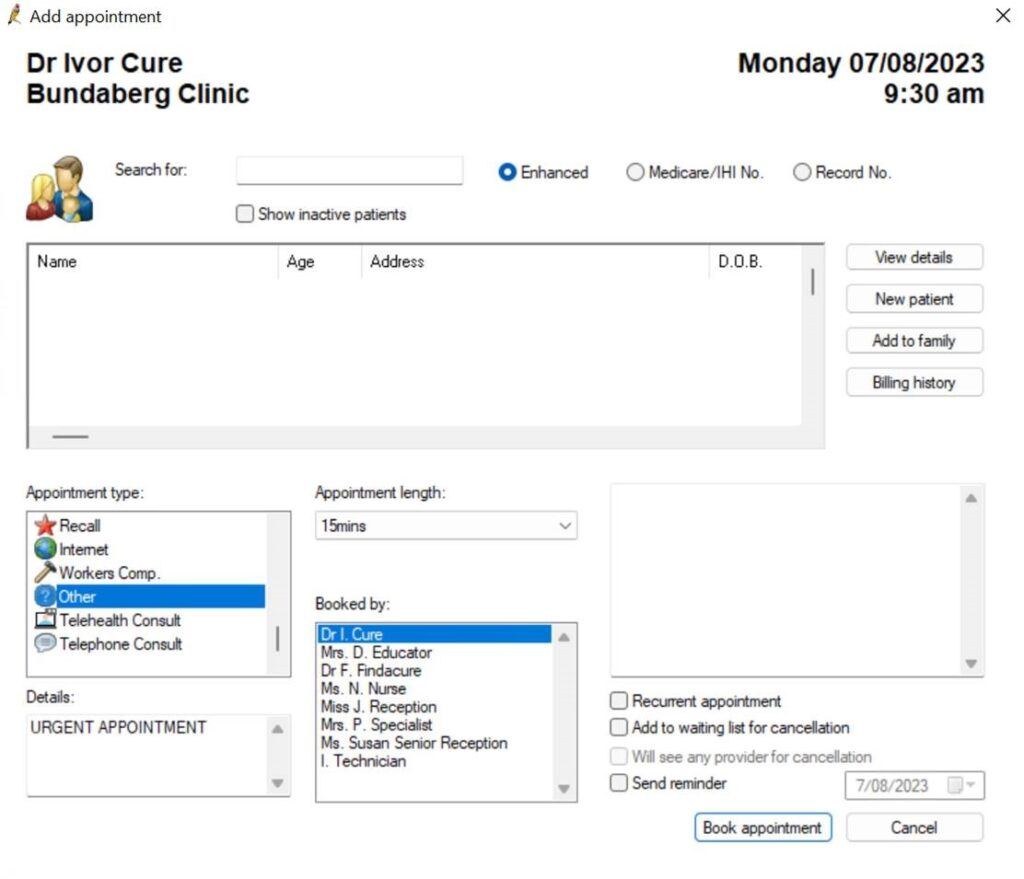
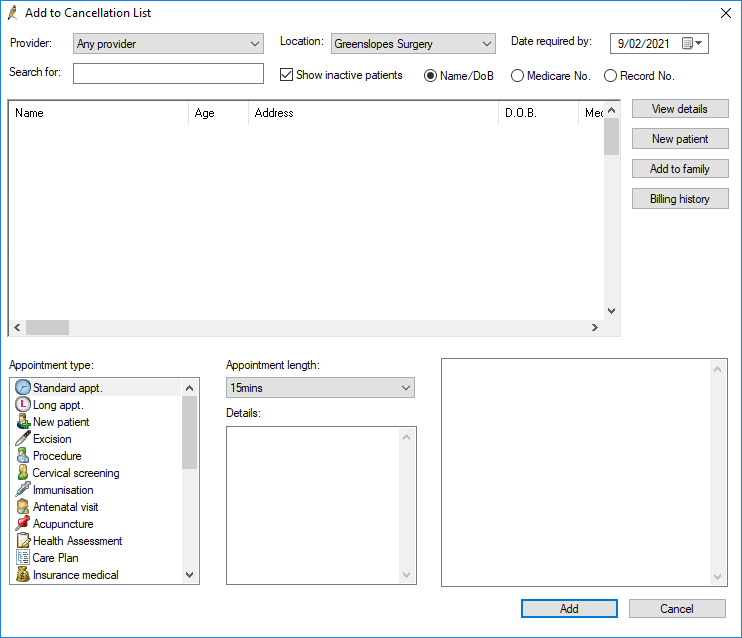
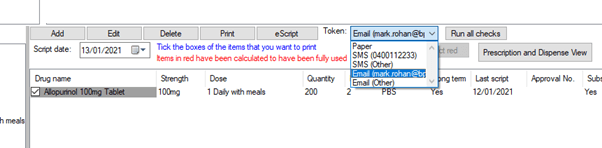
Bookings in an instant: Real-time visibility in the Bp Premier appointment book for your team and in Best Health Booking for your patients means that there is less chance of a double booking happening – no matter where someone is entering it into the system. This also reduces the burden on your reception team.
Spend less time on admin: By simplifying your practice’s booking workflow and streamlining your practice-patient communications, Best Health Booking helps you spend less time on administrative tasks, and more time on looking after your patients.

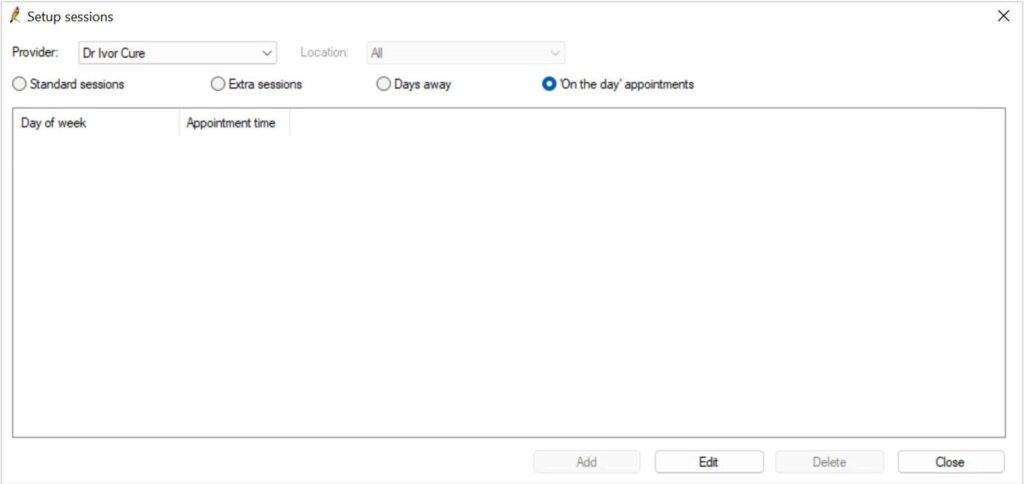
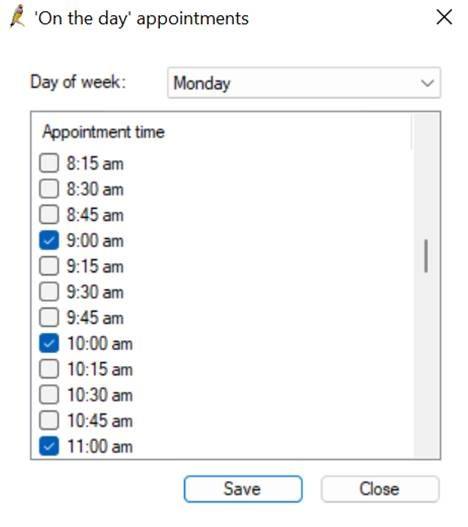
Be up and running in minutes: Once the Best Health Booking Site Manager has been installed, your practice profile can be configured and live in minutes, allowing your patients to instantly book their online appointments.

Bookings anywhere, anytime: Patients aren’t always able to book an appointment on your schedule. Best Health Booking lets them book an appointment on theirs. Your practice’s unique link allows patients to book an appointment 24 hours a day, 7 days a week – no matter where they are. With freedom and flexibility over their health journey, patients are more likely to attend their appointments.

Part of the customer-centric approach has been to keep Best Health Booking pricing as affordable as possible, to support the critical operations of valued practices at the forefront of healthcare in Australia.
We believe that Best Health Booking pricing should be simple and transparent. This means that no matter the size of your medical practice, you will have access to all the features we offer, without paying extra for each one. Our goal is to make it easy for you to subscribe and focus on what really matters – providing the best healthcare to your patients. For a breakdown Best Health Booking pricing, visit https://bpsoftware.net/best-health-booking-pricing.
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars