Welcome to our Employee Spotlight series, where we introduce you to the hardworking and talented individuals who make up TeamBp!
If you have recently been to an industry-based panel discussion, you may have heard the name Danielle Bancroft. Danielle is the Chief Product Officer at Best Practice Software, a Non-Executive Director at Halo Connect, a Co-Chair at the Pharmaceutical Society of Australia, and a practising Pharmacist.
Having worked on multiple large-scale digital transformation projects, including the implementation of real-time prescription monitoring and the national ePrescribing rollout. It’s no wonder why she has now found herself with a vested interest in interoperability and the ecosystem of health tech here in Australia.
The Australian Digital Health Agency describes interoperability as ‘information that has a consistent meaning and how we move it between people, organisations and systems.’ The challenge we face here in Australia is that our healthcare system has evolved over decades without the forward planning of interoperability. Different clinicians, professions and jurisdictions have developed their own ways of working and different technological solutions to support them. This can make it hard when patients move across different parts of the system or when a clinician wants to understand a patient’s history better.
Recently, I sat down with Danielle to learn more about her as a person and chat about all things interoperability.
If you had to pick a song that would play every time you entered a room, what would it be?
Rick Rolling. It started as an April Fool joke in a 4chan chat and became a viral sensation. So basically, you get sent something and think it’s one thing, but when you click on it, it’s actually Rick Astley singing ‘Never Gonna Give You Up’.
One of my previous colleagues also owned a pharmacy. He was one of our beta testers, and we loved ‘Rick Rolling’ him. We sent out a news link through the news channel, and when he clicked on it, it would take him to Rick Astley singing ‘Never Gonna Give You Up’. There’s a whole bunch of these videos on Instagram at the moment. They’re hilarious.
It’s not the actual song that matters. That’s irrelevant. You think you’re going to get one thing, but when you click on it, you get something totally different.
How do you like to spend your weekends? Do you have any hobbies or special interests?
It depends on how much time I have, but I do like to go mountain biking. I tend to mountain bike in the summer, and in winter, I like to go skiing if I can get up to the mountains. I always go to the gym. The first thing I do on Saturdays is my workout. I’ve been doing a little bit of powerlifting lately. And other than that, I’m just very into food. If there’s stuff on, we try different restaurants, lunches, and dinners.
What drew you to want to work here at Bp?
I like to challenge myself to learn new things and grow. I’m fortunate to have worked with someone previously who can come up with an idea and make it a reality. But to meet someone who can do it twice, who knows the customer, that can go and build a product that matches what the customers need twice and makes it successful is someone that I want to learn from. That core aspect of Frank (Pyefinch) is just who he is. He’s so ingrained in understanding his customer.
Balancing that with both Frank and Lorraine in the time that I’ve interacted and worked with them on various projects, they’re the kind of people you want to work for. They’re very honest and down to earth. They care about their customer, but they equally care about their staff.
When did you discover that there was an interoperability problem to be solved here in Australia?
My mother was quite young when she was diagnosed with cerebellar ataxia. It’s been a really interesting journey supporting her from the family side. She has to go to the physio, she gets speech pathology, she goes to her specialist, she has a GP, and none of her records are available across the sectors. So, a lot of the time, my dad has to remember, write it out or get printouts. There are delays in getting the data across to the other professionals. It’s far more complicated than it needs to be.
After working on the ePrescribing side, it baffles me. It’s never been a technology problem. It could be built tomorrow. There’s a collective of issues that stop interoperability from happening, but we’re getting to a critical turning point where we need to get it done. Because ultimately, what is suffering at the moment is the patient.
Where does your passion for interoperability come from?
A need for timeliness and accuracy of patient care. From a clinician’s side, the frustration, there’s no reason why you shouldn’t be able to at least see the data in real time.
Hospital admissions is a key one. The delays are caused when you don’t know what medications your patient is taking. Let’s say that they’re unconscious when they come in, you can’t ask them the questions. You don’t know. Sometimes all you get is a dump of what was in the medicine cabinet from the ambulance. It causes critical delays that could impact the outcome for the patient.
I would like to see it resolved in my lifetime, and I think that it can be done. Fundamentally for me, it’s not about competition or competitive advantage. Collectively, if we all put effort into making interoperability work and having data that we can freely exchange for the patient, we all end up better off, commercially and clinically.
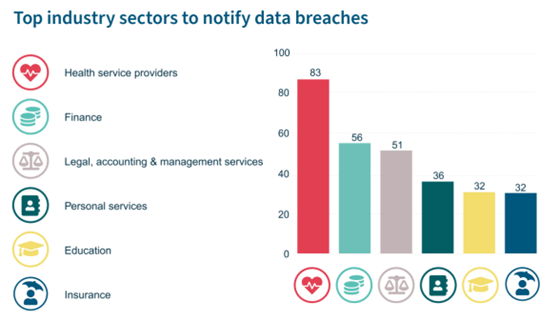
I’m very wary of anyone who enters into a marketplace and calls themselves a disruptor. Genuine disruptors don’t need to tell people that’s what they are. Because health is an interesting one, where you need balance, yes, we want to move forward, and interoperability should be successful. There’s no reason why we can’t make it happen, but that shouldn’t be at all costs. You can’t do that and not make sure that you have adequate security and privacy in place for the patient to ensure that they’re still in control of their privacy to make sure that there’s a certain degree of quality in the applications being offered and that there’s some governance there. I think that’s why it’s always been put in the ‘too hard’ basket because you can’t just simply make it happen. You need structure and framework to make sure it’s being done in the best interest of the patient.
What drew you to want to work with Halo Connect?
The reality is Best Practice has an on-premises product that services a large percentage of the Australian market. It’s no secret that we’re also in the process of re-platforming our products for long-term modernisation. Part of that (modernisation) is how you provide an environment for your third parties. Putting in an API that services all of our products really helps us continue to build our future products while supporting our current existing products and supports our partners in all aspects.
The alignment with Halo Connect purely comes down to why they were doing it and what they were offering. It’s a true partnership in terms of working with Chris (Smeed). His reasons for doing it are about the practice as well as the patient.
Minimising the impact on the on-premise software, there’s all this stuff that you have on the server, all these integrations, how can we make that better so that the clinic can function and focus on the patient and not worry about hardware having pressures and supporting all that kind of stuff.
But also, how do you support the partners to ensure that new market entrants can enter? I think often there’s a high cost to have to connect to every on-premises clinic in Australia. You have to deploy and adapt to each one and have a support desk; it’s a lot of resources. Some small companies might have some really fantastic ideas but not enough funding to enter a market of on-premises software.
Being able to provide a central platform that provides an open marketplace that allows anyone to connect and securely provide information. Halo will offer security and privacy management as it’s an extra layer away from the clinic. It can provide throttling and all kinds of things that actually help the clinic keep their database performance and abstract that layer away. But also provides the ability for partners to connect at a lower cost than having to build their own adapters and deploy them.
It was really about the alignment; they were after the same end goal that we were and for the same reason.
Thank you, Danielle, for this wonderfully insightful chat. From a patient perspective, I look forward to seeing the remarkable work that you are doing in this space and what is to come next.
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars






 When questioned on the Hippocratic Oath, many people will quote the quintessential phrase where the physician promises ‘first do no harm’. One of the more poetic lines from the Oath, however, which very few people would recognise, encourages those in medical practice to, ‘remember that there is art to medicine, as well as science.’
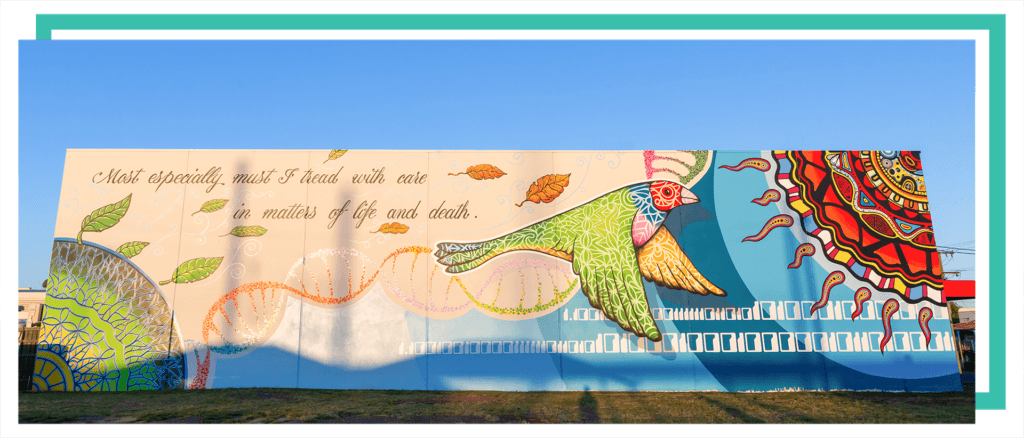
When questioned on the Hippocratic Oath, many people will quote the quintessential phrase where the physician promises ‘first do no harm’. One of the more poetic lines from the Oath, however, which very few people would recognise, encourages those in medical practice to, ‘remember that there is art to medicine, as well as science.’ Best Practice Software is proud to share our special story in the format of this hand-painted mural, which celebrates the story of how Dr Frank & Lorraine Pyefinch developed and grew the idea of creating an electronic medical practice record into one of Australasia’s most successful Health Technology groups. Lorraine Pyefinch shares that the mural illustrates, “the transformation from when doctors had to write everything by hand to a more modern use of automation and technology.” But above all else, it represents the spirit of innovation and its personal connectedness with Health Practitioners and Patients.
Best Practice Software is proud to share our special story in the format of this hand-painted mural, which celebrates the story of how Dr Frank & Lorraine Pyefinch developed and grew the idea of creating an electronic medical practice record into one of Australasia’s most successful Health Technology groups. Lorraine Pyefinch shares that the mural illustrates, “the transformation from when doctors had to write everything by hand to a more modern use of automation and technology.” But above all else, it represents the spirit of innovation and its personal connectedness with Health Practitioners and Patients.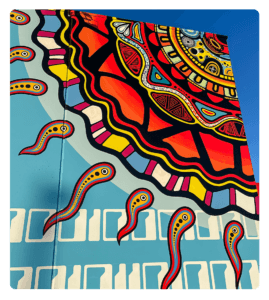 Nicole, as a local Gooreng Gooreng and Bundaburra Yidinji Woman, wanted to “give an Indigenous perspective to the story of the mural.” She brought to life the “Ginmine” (the Sun) as the giver of all life, with science providing its connection to evolution on Earth, and spiritually how it explores and brings light to unseen energies in all living animals and plants. She also incorporated a tribute to the Rainbow Serpent for the significance it plays in creation and the stunning imagery of the beginning of time and greater movement in the cosmos.
Nicole, as a local Gooreng Gooreng and Bundaburra Yidinji Woman, wanted to “give an Indigenous perspective to the story of the mural.” She brought to life the “Ginmine” (the Sun) as the giver of all life, with science providing its connection to evolution on Earth, and spiritually how it explores and brings light to unseen energies in all living animals and plants. She also incorporated a tribute to the Rainbow Serpent for the significance it plays in creation and the stunning imagery of the beginning of time and greater movement in the cosmos.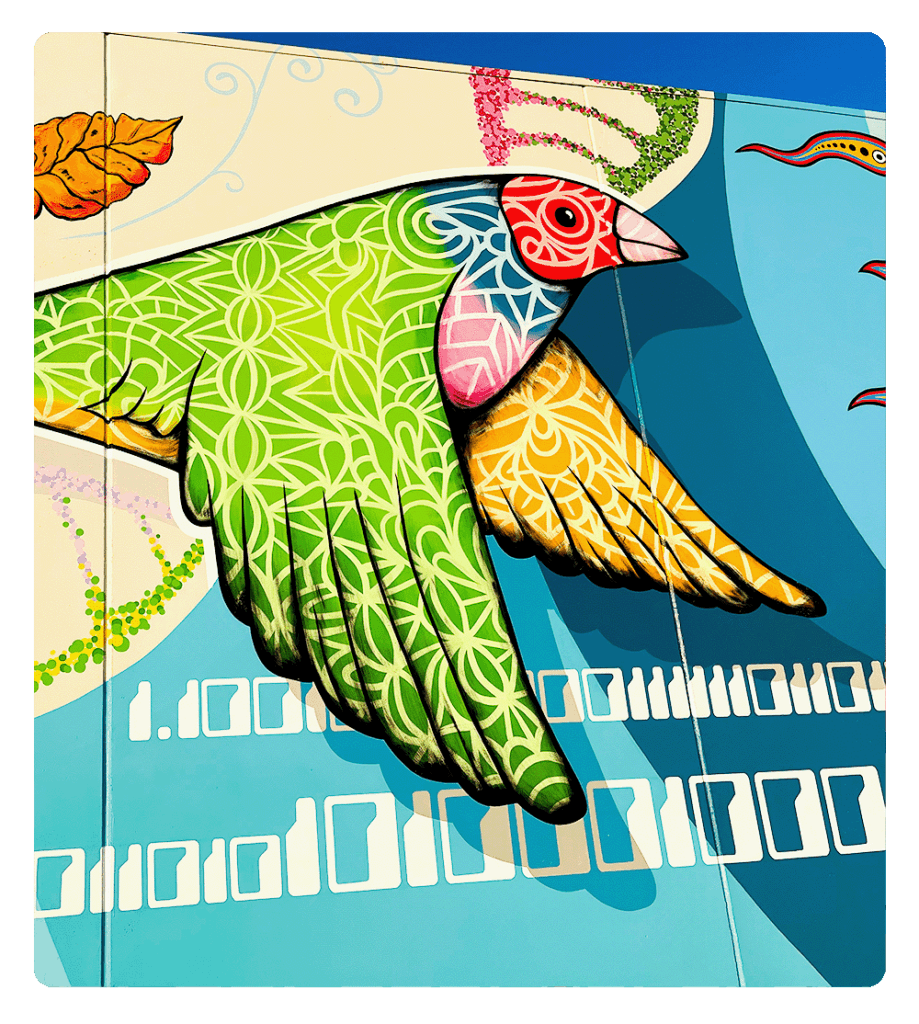 Dr & Mrs Pyefinch’s personal stamp on the quality and interoperability of our software products is represented by the mathematical symbol for “Pi” and the Finch bird (together, as Pyefinch), which soars high above. The Finch connects life between the earth and the sun, and how DNA strands interconnect all we do in supporting Healthcare Practitioners
Dr & Mrs Pyefinch’s personal stamp on the quality and interoperability of our software products is represented by the mathematical symbol for “Pi” and the Finch bird (together, as Pyefinch), which soars high above. The Finch connects life between the earth and the sun, and how DNA strands interconnect all we do in supporting Healthcare Practitioners