As a healthcare professional, you understand the importance of managing paperwork and patient documents. You would know how challenging this ongoing task can be. It’s an essential daily responsibility that can quickly consume your valuable time — time that could be spent in patient care. It can be tedious, but it’s a necessary part of the job.
Documentation is an essential component of effective healthcare communication. Given the complexity of healthcare and the fluidity of clinical teams, patient documents are one of the most important information sources available to practitioners. Good documentation improves patient outcomes by enabling information exchange and continuity of care by all healthcare team members.
When practice staff upload medical documents, there is always the risk of human error. The document upload process is repetitive and regularly interrupted by patients, phone calls, or colleagues. Admin staff often find this task boring and repetitive making it more likely for them to lose attention. The chances of making a silly little mistake are high – incorrect patient search, selecting the wrong document to be uploaded, and hitting the delete button while uploading are examples of where it can go wrong. This can result in uploading the wrong document into the wrong patient file, which can have serious medico-legal ramifications for doctors and medical practices.
All too often, when files are lost or misplaced, practice staff will spend hours looking for the correct document. This can result in calls to other providers requesting these documents be resent. This time-consuming process happens at the practice’s expense, resulting in patient appointments needing rescheduling and a bad reputation for the practice’s document-handling process. Lost files can also be a safety and quality risk, particularly at transitions of care where there is a higher risk of information being miscommunicated or lost.
GP practices deal with highly sensitive information daily. Little mistakes in documentation upload can lead to significant adverse outcomes in the future. Document management solutions are more than just vaults for securely storing healthcare information. They are dynamic tools that allow for safe and effective collaboration as documents evolve.
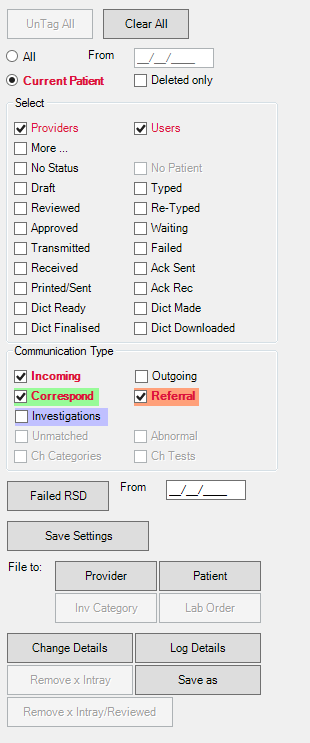
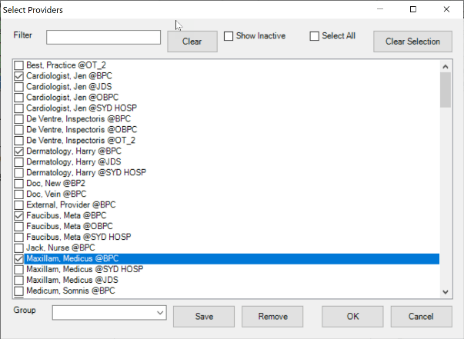
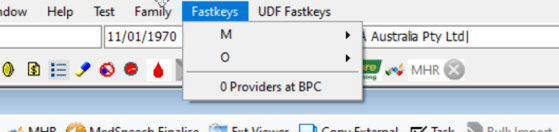
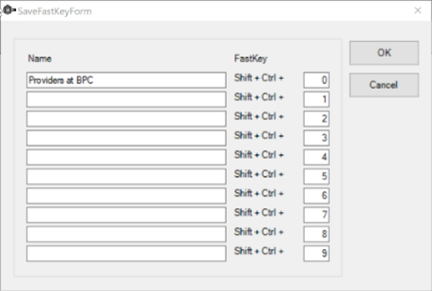
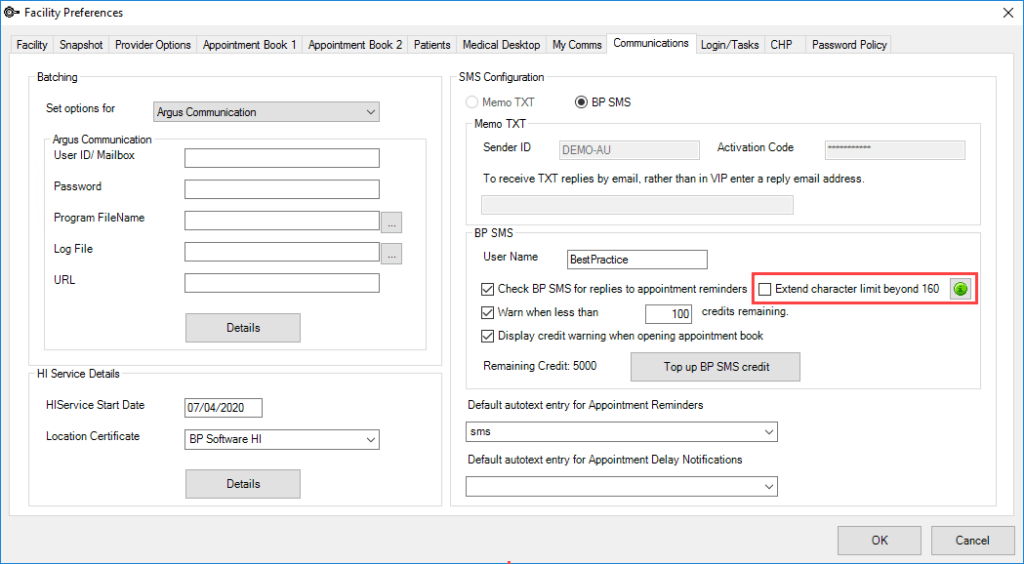
The medical document upload tool, OCR (Optical Character Recognition), can upload any file landing in the doctor’s investigation inbox, elevating the burden on staff to sort and upload manually. It is a widespread technology that recognises text inside images, including scanned documents, PDFs and photos. OCR technology converts virtually any image containing written text (typed, handwritten, or printed) into machine-readable text data. The OCR tool can perform an exact match of the patient’s name, date of birth, address, and other identifying details, then sort the documents into their appropriate files as they are received. Saving your practice time and resources that would otherwise be used to manage unsearchable data.
Click here to learn more about how the OCR tool can work for your practice, or arrange a free demo.
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars