The RACGP Practice Owners Conference for 2021 took place in Brisbane on the 19th and 20th of June. The event was incredibly educational and covered a breadth of topics, all presented by a diverse panel of thought-provoking experts in their respective fields.
During the first day of the conference, I was able to attend sessions on the following topics:
- The evolution of a consumer-driven primary care clinic
- Developing KPIs for your Practice
- How to optimise your outcome from a sale or partial sale
- Using product thinking in general practice to create a successful clinic for the future
- Using data to improve business efficiencies and patient outcomes
- Medical compliance; an overview
- How to structure your Practice & premises purchase
- How to unlock the value of your Practice
- Digital tools of the trade
- Marketing digital strategies
The Future
The future of healthcare will need to be:
- Individualised
- Intelligently designed to enable successful patient outcomes
- Co-ordinated
- Co-joined
- Compassionate and respectful
Practice Challenges
The five biggest challenges Practice owners face are:
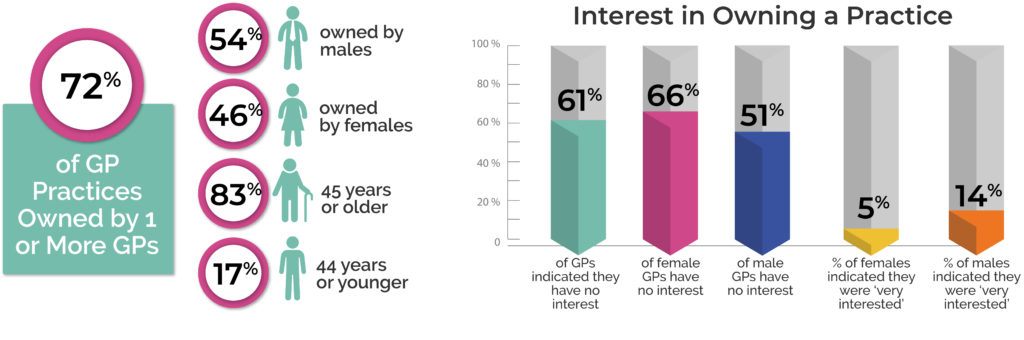
- General Practitioner availability
- Practice revenue is not keeping up with increases in costs
- Keeping up with constant compliance and regulatory changes
- Remaining competitive in the face of competition
- Finding time to work on the Practice, when they’re not working in it
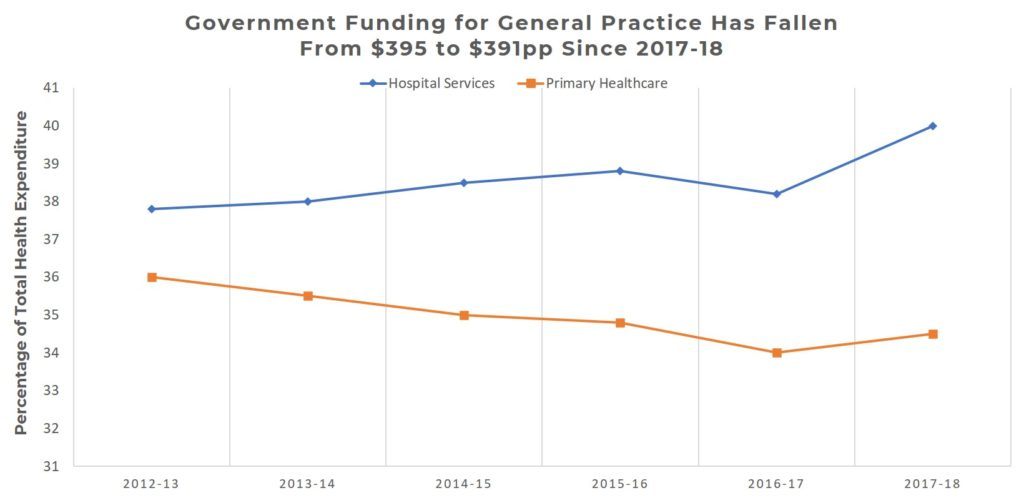
Economics and Financial Health
Practices have three main methods in which they can drive profits:
- They can sell more
- They can charge more
- They can pay less
Here are some interesting statistics to do with maintaining the financial health of a Practice:
- Practices will typically charge 35-45% of their GPs gross takings
- The typical net profit margin for a clinic is anywhere from 2-7.5%
- Non-doctor revenue can be between 16-19%
- A solid staffing ratio for Practices is 1 GP : 0.4 Nurses : 0.9 Admin staff – from this, how are Practices ensuring that their workforce is optimised based on the number of practicing GPs each day?
Marketing Position & Ease of Doing Business
Clinics need to understand their position in the market and their business models. This is especially important with regards to scale vs specialisation. There are a number of levers that clinics can utilise to differentiate themselves in the market:
- Price
- Speed
- Convenience
- Patient experience
- The reputation of individual doctors
- Being a ‘one-stop shop’
- Proximity to retail outlets
- Community connections
- Ease of accessibility
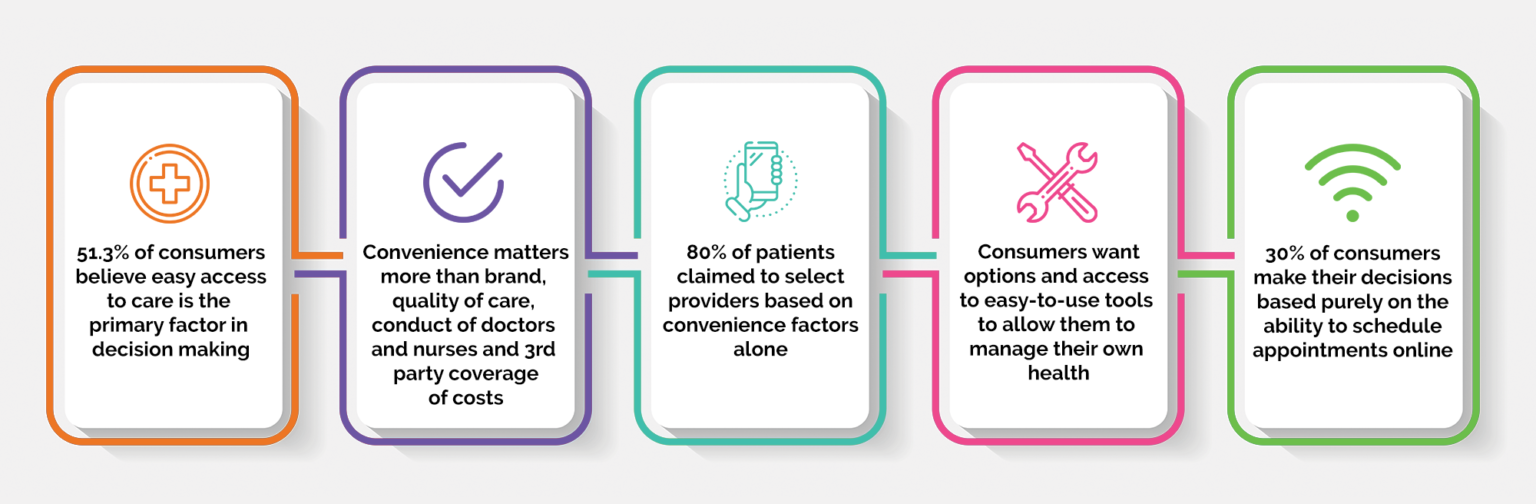
It is also important for Practices to consider how easy it is for patients to do business with their clinics. To accurately assess this, Practices need to understand their current end-to-end patient journey, ensuring they are meeting their patients’ evolving needs. This is something we covered in a recent blog article on the topic of Healthcare Consumerism.
It’s critical for Practices to remember that it is much easier to improve their service for existing customers, than trying to capture new ones.
Understand Your Customer
A key theme present at the RACGP Practice Owners Conference was that Practices need to ensure that they understand their customers.
What problems are your customers facing? Of these, which are the most important? Do you have a solution to these problems? It is recommended that Practices regularly validate and test their hypotheses on how those problems can be solved.
A strong indicator that you have a good understanding of your market is when you are receiving positive recommendations, and have a healthy number of sale volumes.
Above all, Practices need to remember that they can’t be all things to all people. Decide early on which segments of the community you’re trying to service, and focus on those segments.
Measuring Success
Measure the metrics that matter to you, while ensuring that those metrics are practical and support your business model. In addition, don’t misallocate your KPIs, and always make sure that there is a clear link between your targets, and how you measure them.
When considering metrics for success, many Practices focus on the past. This isn’t always helpful, as you can’t change the past! Focus on what needs to be changed for the future, and how you can measure the progress towards those objectives.
When measuring success, break your business down into parts. Ask yourself the following questions:
- How profitable is each part?
- Is each part worth doing?
- How can one area of the business support another?
- Are we using appropriate benchmarks? (are you comparing apples to apples? or apples to oranges?)
- Pilot initiatives and measure their effectiveness. If those initiatives are delivering success, persist with them. If not, stop and reassess, then pivot
Use Data to Drive Positive Outcomes
It’s critical that Practices know where their data is coming from. A Practice can generate value from triangulating Practice, financial, HR/Rostering and MBS data.
However, not all data is equal. Just because the data is there, does not mean it’s going to be insightful in developing Practice value.
According to an interview with Cubiko, here is a list of what data Practices will want to track:
- Total number of billings (vs the Practice budget)
- Average wait times (week-on-week)
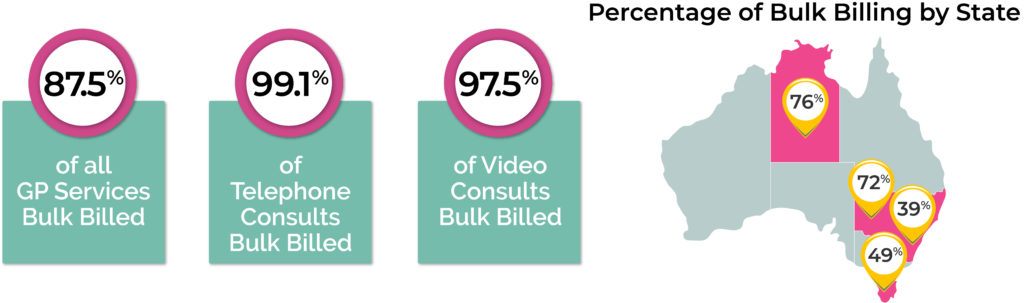
- Bulk billing (week-on-week)
- Utilisation of appointments – booked vs available vs admin
- The number of appointments vs billing – ideally in a 4×4 matrix
- Last week vs forecast with regards to recalls and reminders, and telehealth
- Room utilisation
- No Shows
- The cost of each appointment and net profit from billings, more specifically:
- Don’t always look backwards at what previous appointments have cost you, look forwards to what appointments are going to cost you
- How much of your diary is booked? If you have large gaps between appointments, consider why
- Look at your roster of doctors, and consider your ratios to nurses and admin staff. Does it make sense?
- Benchmarking – internal benchmarking is powerful, If possible, find a sister Practice that is similar and partner with them to benchmark your performance. Make sure you’re comparing apples to apples!
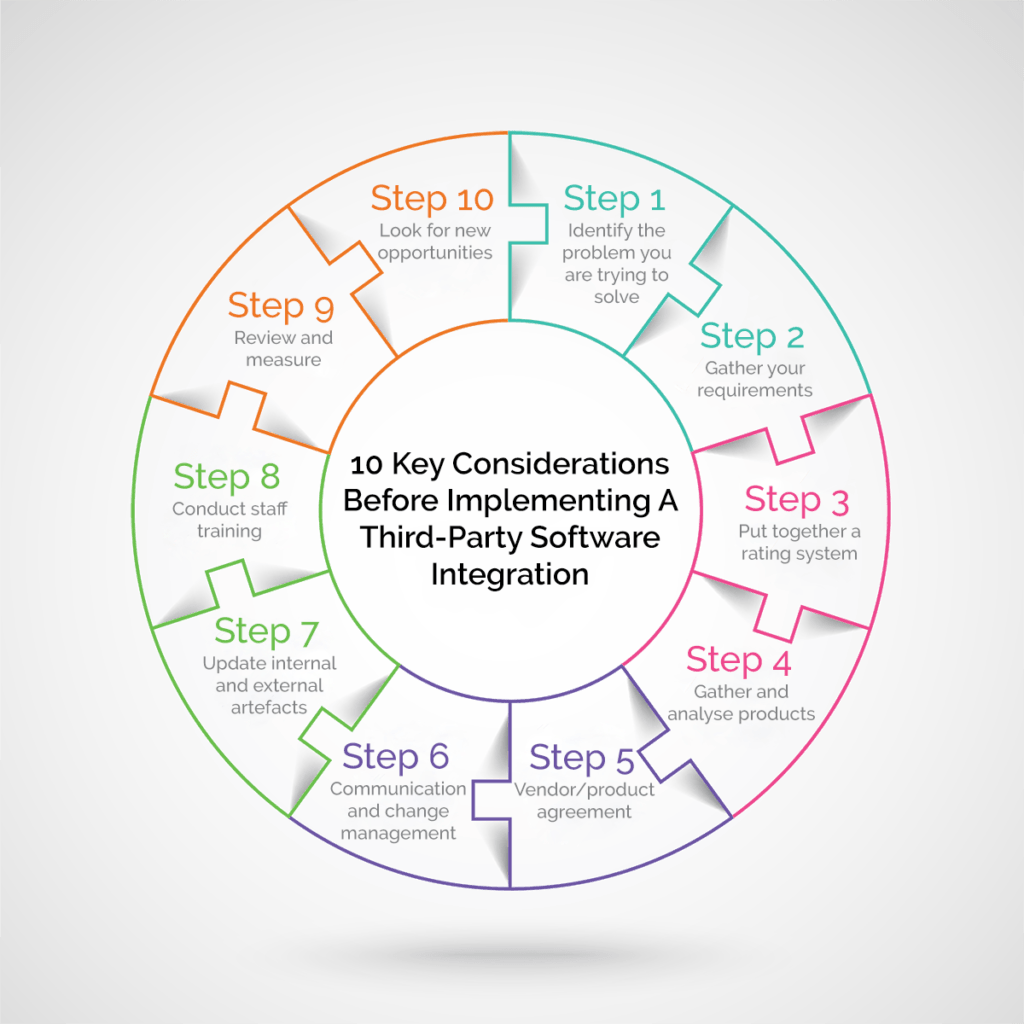
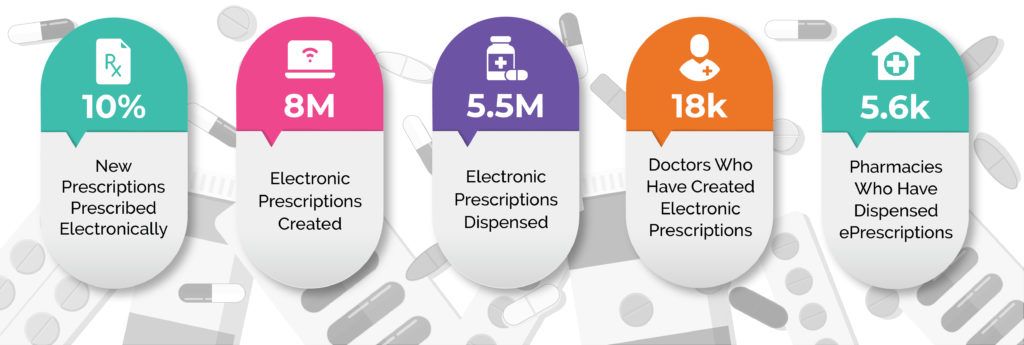
Consider Your Technology as a Tool of the Trade
Recent trends have shown that patients want greater control over their data. Practices need to better utilise digital tools to engage with their patients.
- Websites – Have they had their day? Make sure your Practice website is designed for your patients, and not focused on your business
- Social Media – Platforms like Facebook and LinkedIn are great mechanisms to connect with peers and share your business best practices, helping you to work towards positive patient outcomes. Social media is also a great tool to gauge market sentiment
- Telehealth – How do we leverage telehealth for follow-ups? Telehealth has given us an opportunity to forge our future on how to better interface with patients. For example, can telehealth be used by metropolitan Practices to support rural sites?
- My Health Record – GPs were once the custodians of their community’s medical records. Now, that data is available for people to control. As an example, mothers and fathers can now help in their children’s journey – this is especially true for initiatives like the NDIS.
- eOrdering – Coming soon, and coming quickly. Pathology and radiology providers are coming online and enabling eOrdering. Patients receive an electronic token, and the tests go straight back to the GP.
- What else is on the horizon?
- Provider Connect Australia – A new system that, once information is entered, will be a single point of reference. However, service directories have been an issue in the past.
- Home Monitoring – Is virtual care something that’s in the future?
The RACGP Practice Owners Conference provided attendees with some incredibly valuable information for the present and future of the healthcare industry in Australia.
The past few years have been unprecedented in how global events have impacted healthcare, and now more than ever it’s crucial that Practices take control of their businesses and ensure viability and success for the years ahead.
Authored by:
Peter Polacek
Product Manager at Best Practice Software
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars