In comparison with other countries, Australia’s COVID-19 vaccine rollout plan was very measured, and the implementation has been somewhat leisurely. With the frequent changes to the guidelines paired with vaccine hesitancy, vaccination hubs and GP clinics around the country have faced many challenges in their quest to immunise the nation.
In theory the government’s plan was considered and robust – vaccinations would be done in phases, where the most vulnerable would be immunized first, and the young and healthy would be immunized last. Millions of doses of the Astra-Zeneca vaccine were ordered, and could be manufactured locally, while fewer of the more expensive Pfizer vaccine was ordered for the most vulnerable.
A central online system was developed that allowed citizens and residents to determine which phase of the rollout they qualified for. Those who qualified for the first phase, aptly titled 1a, would be vaccinated soonest with the Pfizer vaccine at government run vaccine hubs. Those who were 1b or lower in the schedule could book into a participating GP clinic near them to get the Astra-Zeneca vaccine.
Anyone who was involved with the logistics, patient booking, ordering and administration of COVID-19 vaccines was required to complete a five hour online module developed by the federal government to ensure adequate and uniform training of all personnel involved in the vaccine rollout. This included couriers, receptionists, nurses, doctors, and Practice managers at GP clinics around the country.
The plan also involves recording the vaccination details in a centralized system, the Australian Immunisation Register. A lot of groundwork had to be done by software vendors to enable the seamless uploading of this data. This data would help to accurately determine how many people have been vaccinated, in addition to enabling the safety of vaccine administration to ensure they are administered within appropriate time frames. Reactions to vaccines are also being collected to track trends and monitor for any emerging serious reactions.
Despite Australia’s COVID-19 vaccine rollout plan, four months into the rollout, as of the 3rd of June only 4.6 million vaccine doses have been administered in Australia, with only 2.1% of our population being fully vaccinated against COVID-19. A rough comparison with other countries with a similar GDP per capita and healthcare systems, over a period of five months paints a startling picture:
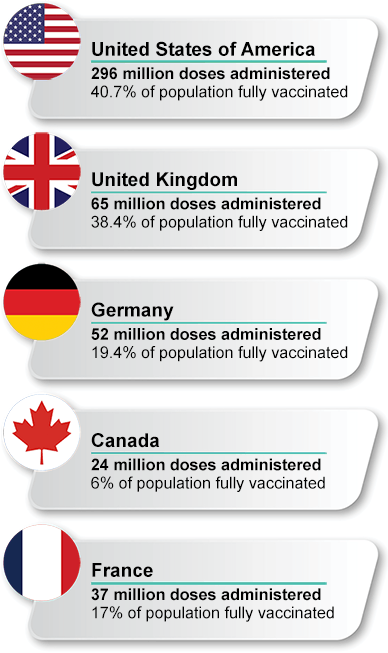
The large vaccination numbers in the above-mentioned countries are mostly likely a reflection of the disastrous effect COVID-19 has had socially and economically in those nations, resulting in a more urgent rollout and vaccine acceptance within the community. Given the low level of infections and community transmission in Australia, the immediate benefit of the vaccine is not overtly obvious to many Australians and so the uptake has been slow.
Now with yet another outbreak in Melbourne, a sense of urgency has re-emerged as the public realise the pandemic is still very much a risk to us and this could happen anywhere in the country. Despite the risks of the vaccine, it is clear now from data overseas that the benefit is still greatly outweighed. One of the most common concerns held by those who are vaccine hesitant is the risk of blood clot from the Astra-Zeneca vaccine. Recent Australian data shows 31 confirmed cases of thrombosis with thrombocytopenia syndrome and 10 probably cases, out of a total of 3.29 million doses administered. At the time of writing, the death rate remains at one. Conversely, for every million people diagnosed with COVID-19, 165,000 of those cases (16.5%) experience blood clots as a symptom of the virus.
On the 1st of June 2021, the UK saw its first day without a COVID-19 death. This is a remarkable feat made possible due to their extraordinary vaccination rollout. Similarly, the USA has also seen a significant reduction in mortality and morbidity. Meanwhile other countries, such as Japan, that initially had a slow rollout and low vaccine uptake, are ramping up their vaccination efforts after recent Covid-19 outbreaks.
As a GP who is involved in vaccination counselling and administering the Astra-Zeneca vaccine, the experience has been interesting. From discussing patient concerns, to ensuring informed consent, appropriate documentation, and counselling on the potential side effects in a very short consult has been challenging. There is an immense amount of paperwork and logistical work that is done by my Practice manager and nursing staff to smoothly run the COVID vaccine clinics. Patients are confirmed multiple times to ensure they attend their appointment to avoid wastage of vaccines.
From a funding perspective, our clinic is not making money with this enterprise, but rather we are doing it as a service to the community. For patients, it is much more convenient to have the vaccine at their local and familiar health care centre rather than a large vaccination hub with thousands of other people like we have seen overseas. In some of these centres, both local police and the military have been involved with administering vaccinations.
As medical practitioners we are taught to look at the evidence and what can be deduced from large amounts of data. There is a limited role of anecdata in medicine, yet I still do get asked “What did you do doc? What has been your experience? Is your family ok?”.
I had registered myself to get the Astra-Zeneca vaccine. Despite being considerably concerned about the risk of thrombosis with thrombocytopenic syndrome, I felt the risk of the sequalae of COVID-19 was much worse. After all, what is the point of worrying about the long-term effects of vaccine related complications if I didn’t make it through the pandemic itself? I ended up having to cancel my Astra-Zeneca vaccination as the guidelines changed, and I have subsequently received two doses of the Pfizer vaccine. Overseas, I have elderly relations who have had the Astra-Zeneca vaccine and have either, at worst, had a very mild infection or, at best, had escaped infection all together.
To get through this pandemic, no doubt we all must work together as no one is safe, until everyone is safe.
Authored by:
Dr. Fabrina Hossain
Clinical Advisor at Best Practice Software
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars