Contributed by guest author, Dr Stephen Jelbart.
Haven’t we progressed since the introduction of information technology! We doctors can do everything so much more efficiently nowadays, compared to the old days of pen, ink and card records. That’s what we like to think anyway, but have we actually improved? Have you really advanced and improved your efficiency in parallel with the IT? Are you keeping up? Did you know that Bp Premier features a range of ways in which you can achieve that coveted efficiency?
Your efficiency in generating patient notes, documents, and referrals is determined by your knowledge, understanding and proficiency in the use of the attributes of the software available.
Most people use Microsoft Word or something similar, but few people utilize the full power inherent in Microsoft Word. Templates, Macros, Tables, Nested Tables etc. Similarly with Microsoft Excel. I like to think that I can use a spreadsheet reasonably efficiently, but I was in awe and flabbergasted when I saw my friend, a chartered accountant, generate a business plan in Microsoft Excel within one hour, when is it had taken me the best part of two weeks to generate something that was not nearly as accurate and comprehensive! Figures, formulae and calculations flowed from his fingers with amazing speed. He generated a cash flow analysis with a simple ‘copy and extend’ manoeuvre that was not only amazing, but horrifying when he pointed out the long-term effects of ignoring ‘getting the cash through the door’. But that’s another story, a blog for the entrepreneurs to pursue!
Bp Premier is, without a doubt, the best general practice software available on the market in my opinion. However, I hope further improvements can be adopted (are you listening, development team?).
ACRRM and RACGP demand that we take detailed and comprehensive notes to cover all bases. It is also “best practice” for indemnity purposes to maintain succinct, accurate notes and this is where agile use of IT can help us do so. Let’s just take a quick look at how the layout in Bp Premier lets you do that easily.
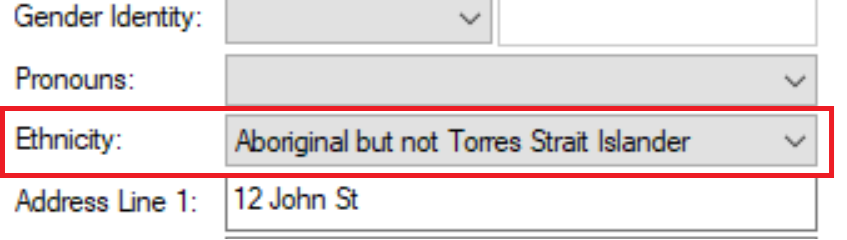
- On the left, at the top corner, you have patient name and address. Double-click up there (or F10) and you access patient demographics. I frequently check to see if all that info is accurate as you don’t want to be sending an SMS, for example, to an incorrect mobile number!
- Moving down sequentially along the left-hand side of Bp Premier, you have the best guide available for ensuring your logical progression through systematic questioning and examination of the patient.
- Start at the top and move down:
- Allergies and Sensitivities
- Current Notes
- Past Visits
- Past History
- Medications
- Immunisations (accurate documentation is now legally very important with COVID-19 shots)
- Family and Social History
- Etc.
It’s all there and laid out in a logical and sensible manner as a reminder to complete a comprehensive examination and history – all extremely important from the dreaded audit and accreditation point of view.
Always Consult Previous Visits
I open this up and quickly scan through the most recent visits to ensure I’m on the right page when the patient comes in. Saves a lot of potential embarrassment.
Past History should, if data has been entered correctly, give you an idea of the current maladies. Make sure you use the database provided when adding PH. Don’t add free text to the main diagnosis – you can’t accurately search for free text entries! If your diagnosis or ‘Reason for Visit’ needs more detail, add that in the comments box at the bottom. Demote resolved issues to ‘Inactive’ to keep the current problems succinct and Up to Date. Make sure you enter the date of diagnosis when adding a problem – otherwise a long-standing history of Hypertension might appear to have been diagnosed in 2021!
The same is true with medications! Always review the medications list to ensure only current medications are included – otherwise any referral will likely contain a long list of pills and potions that haven’t been taken for years.
Next Up - Patient Notes!
Always look at your patient, listen to your patient, interact with your patient – taking time to do so is always well spent as you pick up ‘non-verbal’ communication that can hone your overall assessment. Let the patient talk and help tease out the main issues early in the consultation so that you can prioritise to ensure you address the important issues. Doing this early in the consultation helps to develop an early rapport and avoids that “… and just one more thing Doc” at the end of the consultation which can quickly erode the 15-minute consultation time allocated to your next patient. When you know all the issues, you can get your patient to make another appointment to address the less important problems.
You’ve now spent some time listening and you need to adequately document the consultation. You can save yourself heaps of time using ‘Autofill’. Spend the time to populate all your favorite notes into Autofill initially, and once they are in place you will save yourself heaps of time.
Let’s say your new patient has Hypercholesterolaemia and Hypertension and needs new prescriptions. You might just add those meds to the list, print them out and say ‘goodbye’, and ‘next please’ but it’s valuable for audit purposes to actually document that initial brief interaction. You can type that out long-hand (correcting your spelling as you go) or using Autofill and type:
‘Rpts’ (to generate from Autofill);
“Patient presents for repeat prescriptions” for
‘hc’ (to generate “Hypercholesterolaemia”) and
‘ht’ (to generate “Hypertension”) –
That’s just 14 characters typed to generate 70 characters. Very efficient!
Consider the patient with the common presentation of a mild URTI.
I type; ‘Li’ (shorthand for “Little to find”) and Autofill completes the following:
Patient presents with URTI symptoms for the past ? days.
On Examination:
Little to find.
No cough.
Dry cough.
Throat not red.
Throat slightly red.
No Lymphadenopathy.
Small upper cervical glands.
Chest clear.
No rash.
Then all you need to do is delete the bits you don’t want to ensure you leave the appropriate documentation. That’s two characters to enable 34 words! Not bad, eh? It does take a bit of practice to remember the short-cuts but after a week or so, you’re off and running.
Here’s another:
‘Knex’ (shorthand for Knee Examination)
This Autofill serves as a reminder of the elements of a comprehensive knee examination.
Add / Delete or modify after your examination.
Examination of the Knee: LEFT / RIGHT
Normal gait / limp?
Any swelling or deformity / inflammation
Full and free Range of Motion? Active / Passive
Flexion limited by pain / stiffness to …Full extension?
Patella tap – No effusion / Small effusion
Patella crepitus – present / none
Anterior draw test; -ve / +ve
Lachman test; -ve / +ve
McMurray test for integrity of the meniscus
Tender on palpation? Joint line pain?
Varus and valgus stress to assess collateral ligaments
Pivot shift for ACL; -ve / +ve
So, there are a few ideas with some Bp Premier features to get you started if you haven’t already established a repertoire in Autofill.
Given that many GPs move around a lot nowadays, particularly the Registrars, it would be very handy (once again, development team take note!) to have the ability to download Autofill to a flash card to make all your hard work on developing software efficiency with Autofill, portable for your next Registrar assignment!
Authored by:
Dr Stephen Jelbart
Guest Blog Contributor for Best Practice Software
Dr Stephen Jelbart is currently practising at Plaza Medical Centre in Kalgoorlie, WA.
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars