Real Time Prescription Monitoring (RTPM) is a clinical tool available in most states to practices running Bp Premier that assists healthcare providers and pharmacists in making safer prescribing decisions for certain high-risk medicines. See Real Time Prescription Monitoring availability for more information.
To maintain the highest levels of patient safety, healthcare providers can take key steps within Bp Premier to support and enhance the data quality of the Real Time Prescription Monitoring system.
Validate the Patient's Individual Healthcare Identifier (IHI)
One of the most important steps in ensuring data accuracy is validating the patient’s Individual Healthcare Identifier (IHI) in Bp Premier. Validating the IHI ensures that the correct medical information links with the correct individual. Incorrect or missing IHIs can result in duplicate patient records, risking patient safety and potentially leading to incorrect diagnoses, inappropriate medications, and medical errors.
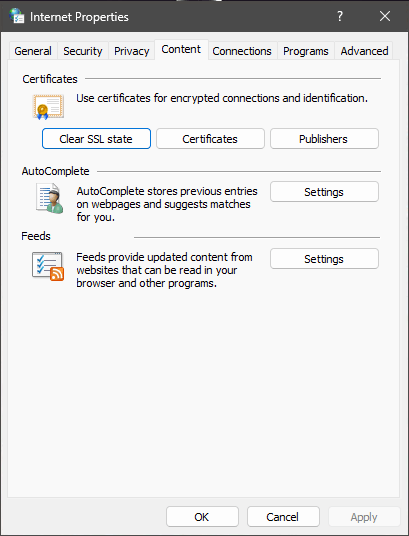
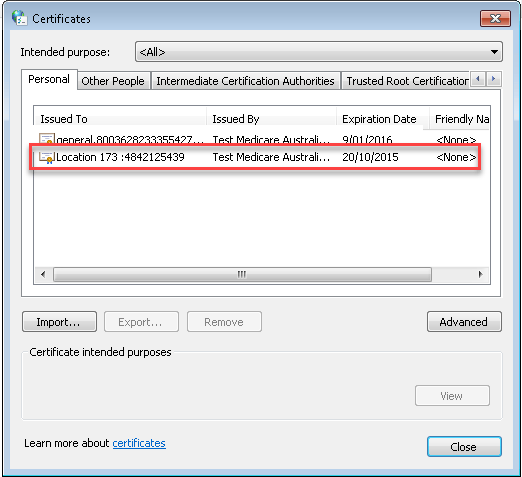
To assist healthcare providers in improving data quality and patient safety, Bp Premier has several functions that simplify validating patient IHI numbers. In Bp Premier version Orchid, we added functionality to automatically validate a patient’s IHI number when opening the patient record. When saving patient demographic information, a prompt will also display if the IHI number is invalid against the new identifying information.
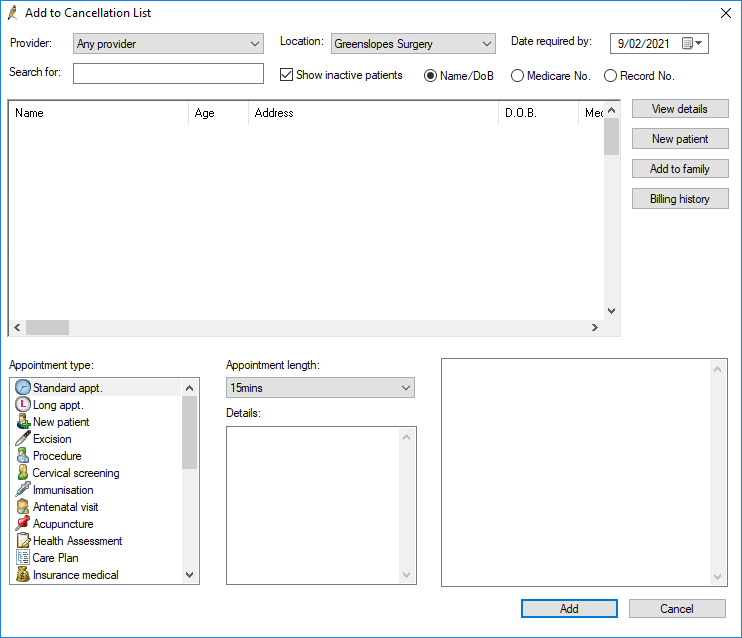
Patient IHI numbers can also be manually validated for a single patient from the patient demographics screen or validated in a bulk lookup for multiple patients from the appointment book.
You can find more information about Validating Health Identifiers in Bp Premier in our knowledge base.
Maintain Accurate Patient Demographic Information
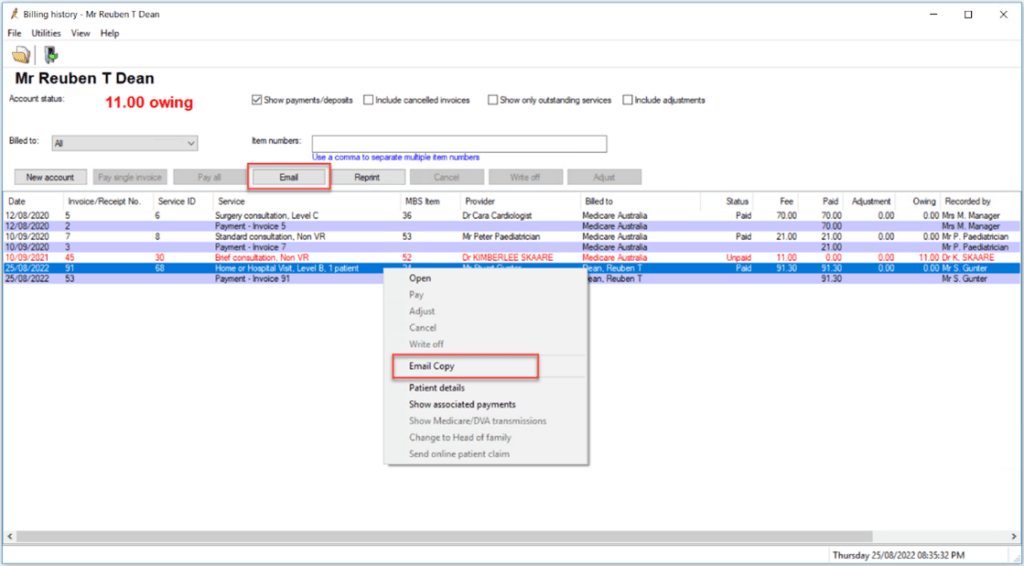
Real Time Prescription Monitoring does not rely solely on prescription and dispensing records; it also gathers patient information from other sections of Bp Premier. To reduce the risk of data inconsistencies, ensure that patient details such as last name, first name, address, date of birth, gender, and Medicare/DVA number are recorded and kept up to date.
Record the Patient's Date of Birth
When prescribing or dispensing medication, healthcare providers and pharmacists must record the patient’s date of birth. For prescriptions containing Schedule 4 and Schedule 8 medicines, the patient’s date of birth is a required data element. Recording the patient’s date of birth also helps ensure that accurate data is retained in real-time prescription monitoring systems and reduces the chance of duplicate patient records.
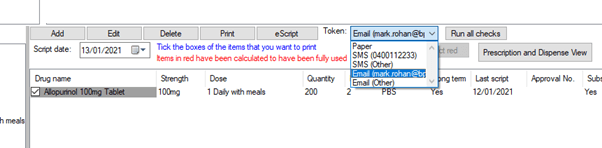
Enter Medicine Information Correctly
Medicines prescribed as free text are more difficult to match in the RTPM system. Healthcare providers should take care when selecting medicines, accurately record dosage and quantity information, and avoid free text entries whenever possible. Real Time Prescription Monitoring relies on the accuracy of this information to generate alerts and notifications regarding at-risk patients.
Real-time prescription monitoring is essential for improving patient safety in the healthcare system. Healthcare providers help improve this tool’s accuracy and effectiveness by actively participating in efforts to improve data quality. Validating IHIs, keeping patient information up to date, and correctly recording prescription information are essential steps in ensuring system quality. By implementing these measures, healthcare providers can uphold the highest patient safety standards while providing more reliable and consistent care to their communities.
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars