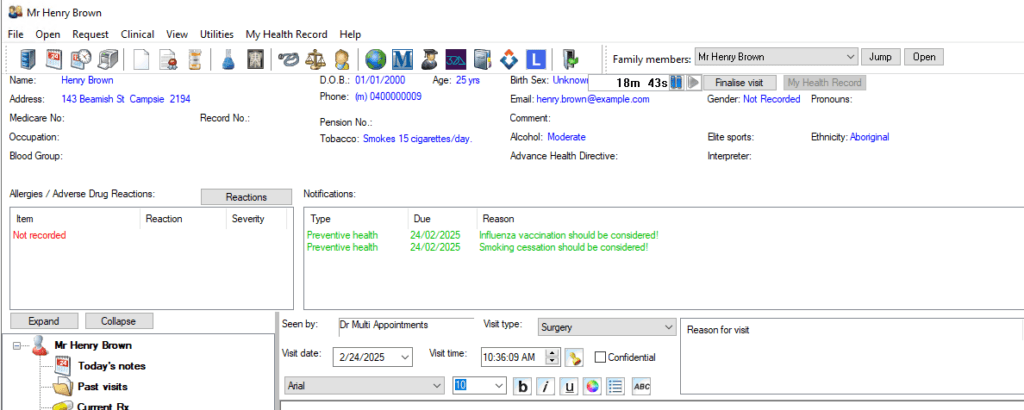
Torres and Cape Hospital and Health Service (TCHHS) provides essential health services across one of Australia’s most remote regions: Torres Strait and Cape York Peninsula. This area comprises 31 Primary Health Care Centres (PHCCs), two hospitals (Thursday Island and Bamaga), a multi-purpose health service (Cooktown), and an integrated health service (Weipa).
Amalgamated in 2012, this Hospital and Health Service (HHS) is responsible for the health services of a population of over 26,000 people covering an area of more than 130,000 square kilometres. 63.7% of this population identify as Aboriginal or Torres Strait Islander. Making this HHS one of Australia’s largest health services providers to Aboriginal and Torres Strait Islander peoples.
TCHHS’s commitment to providing culturally appropriate healthcare services is crucial, particularly given the complexity of delivering healthcare in resource-limited, geographically dispersed, and socioeconomically disadvantaged communities.
In recent years, TCHHS introduced Bp Premier as their primary electronic medical records (EMR) system to address inefficiencies and patient safety concerns related to their existing clinical and administrative workflows.
Background and Challenges
Prior to the implementation of Bp Premier, TCHHS faced several challenges with their previous system. The northern PHCC sites had been using Bp Premier since 2012, while the southern PHCC sites had been utilising an alternative EMR solution for three years. TCHHS aimed for a unified EMR across its network of service locations to improve uniformity, efficiency, and communication between their healthcare providers. However, the EMR currently being utilised by the southern sites posed significant issues, especially in areas of the electronic delivery of pathology results, imaging, referral letters, and clinical communication.
The Decision to Implement Bp Premier
After carefully evaluating several EMR systems, TCHHS decided to extend the use of Bp Premier across its entire network. The decision was driven by a need for an efficient, reliable, and safe system that could seamlessly integrate with their existing processes and improve workflows across remote PHCC locations.
The key factors in choosing Bp Premier included:
- Safety: A system that ensures the secure and accurate delivery of critical patient information such as test results and referrals.
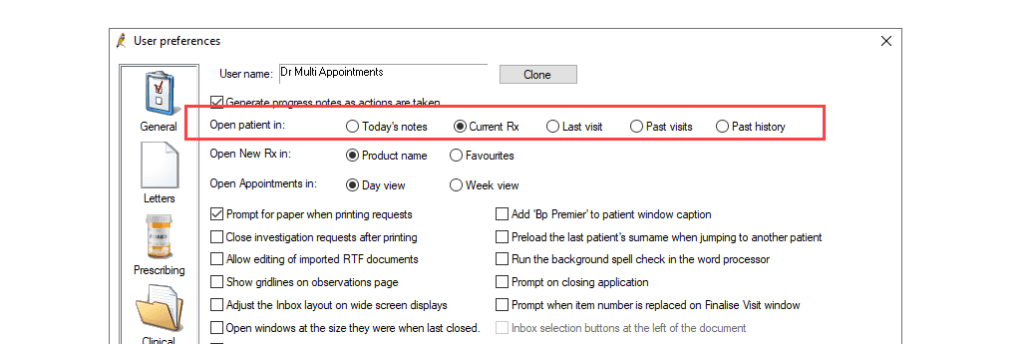
- Efficiency: Streamlined workflows for both clinical and administrative tasks, including billing and appointment management.
- Integration: The ability to unify patient records across the entire health service and populate reports using Bp Premier’s data extraction tools for quality improvement.
- Customisation: TCHHS required a system that could be customised to meet the unique healthcare delivery needs of rural and remote communities, particularly in Indigenous health settings.
Advocacy for Change
Dr Ineke Wever is a GP Rural Generalist with advanced skills in Aboriginal and Torres Strait Islander Health. She is currently backfilling as the Executive Director of Medical Services for TCHHS and assisting with Bp Premier’s continued rollout across the Southern Cape PHCC. Her ultimate goal is to create a single medical record across the HHS.
Dr Wever has been using Bp Premier as her primary EMR system since 2012, describing the solution as “Efficient, safe, reliable and improving primary care workflows.”
She also credits the rollout of Bp Premier with positive impacts on patient safety. “Patient safety has improved, and oversight over clinical follow-up and safety netting.”
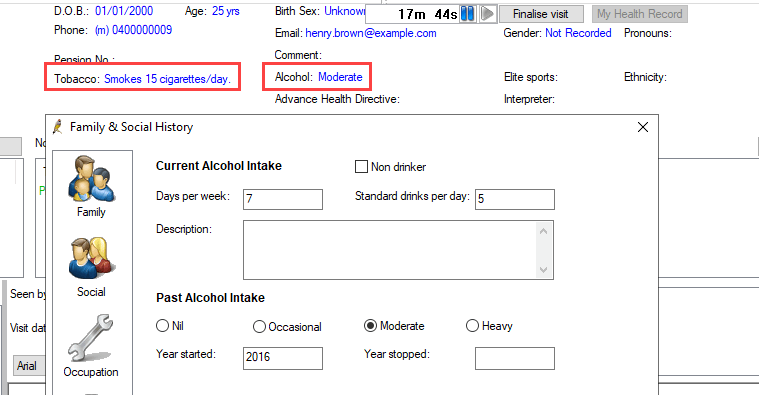
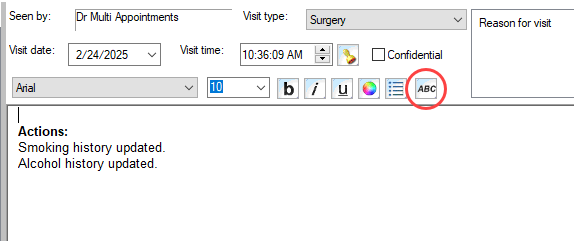
Dr Wever said that the team particularly enjoyed the built-in features of HealthLink SmartForms, John Murtagh’s Patient Education material, observation graphing capabilities, Enhanced Primary Care tools, including health assessments and care plans, plus clinical functions such as the INR manager, cardiovascular risk calculator, DASS21 and Edinburgh PND Scale. The TCHHS has also created customised workflows and templates tailored to their specific service needs.
The Impact of Bp Premier
The rollout of Bp Premier had several positive impacts on healthcare delivery within TCHHS. Some key outcomes included:
- Improved patient safety: Bp Premier ensured the accurate and reliable delivery of pathology results, imaging, and clinical correspondence, reducing patient safety risks.
- Efficiency benefits: Administrative processes, particularly in billing, appointments, and patient recall, became more streamlined, saving time and reducing the burden on staff.
- Customisable workflows: The ability to customise workflows and templates enabled TCHHS to meet the specific healthcare needs of their population, particularly in delivering culturally appropriate care to Aboriginal and Torres Strait Islander communities.
- Reporting and Data Extraction: Bp Premier’s integration with the Primary Healthcare Data Portal allowed TCHHS to extract data for reporting and monitor population health metrics, which is crucial for ongoing quality improvement initiatives.
Conclusion
The introduction of Bp Premier in TCHHS marked a significant step towards improving healthcare delivery in one of Australia’s most remote and untapped regions. The system’s efficiency, reliability and safety have contributed to improved clinical outcomes and streamlined administrative processes. The case of TCHHS exemplifies the importance of tailored, culturally sensitive health solutions in achieving health equity in diverse populations.
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars