As the second wave of COVID-19 continues, clinicians remain acutely aware that the pandemic is far from over. Telehealth consultations and electronic prescriptions were two important digital health measures that helped clinicians provide life-saving support whilst protecting patients and staff against the risk of infection.
Telehealth consultations rose from pre-pandemic levels of 1.3% to 36% of all consultations last year as a result of their addition to Medicare from 13 March 2020. More than 30 million telehealth consultations were performed in Australia throughout 2020. More information on telehealth statistics can be found here, here and here.
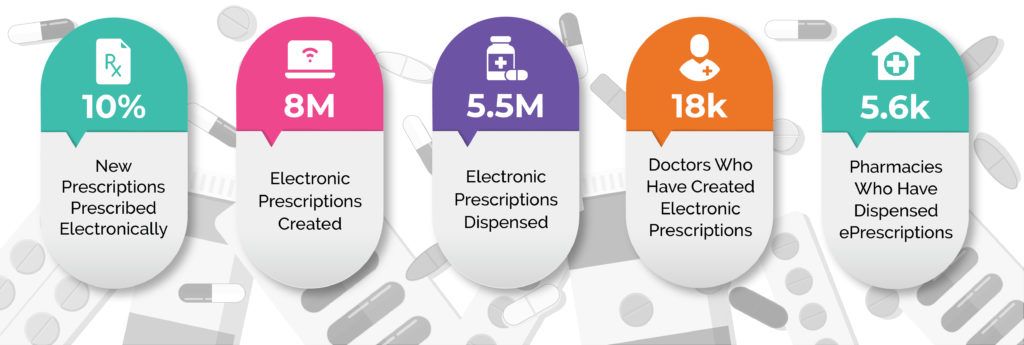
Prior to the introduction of electronic prescriptions in 2019, the patient still needed a paper script. For the past twelve months, as a result of the accelerated national roll out of electronic prescriptions to deal with the pandemic, clinicians have had the option of providing patients with an electronic script via email or SMS rather than a paper script. This provided greater flexibility for patients and reduced the problem of lost or replacement scripts. In the twelve months since, ePrescribing has continued to gain traction, as shown in the following infographic.
Whilst delivering safe, private and efficient prescribing at a distance, Electronic Prescribing has also introduced new clinical benefits. One of the immediate impacts is that clinicians can now cancel an electronic prescription directly from Best Practice Software if the need arises, without having to retrieve the paper script or repeat.
The nation-wide launch of Australia’s first digital script list, called MyScriptList – more accurately referred to as a Department of Health conformant Active Script List (ASL) – also opens up substantial implications for reducing the administrative burden on practices. MyScriptList was launched in partnership by the two national prescription exchange services, eRx Script Exchange and MediSecure. It provides the third national means of access to electronic prescriptions, working alongside the two existing methods of paper scripts and digital tokens (the digitised script sent by a doctor to a patient’s email or phone, introduced in May 2020).
The main clinical benefit arising from the digital script list, or ASL, is that clinicians, patients and pharmacies can now view all of a patient’s current electronic prescriptions and repeats in one digital list. Clinical and administratively, this generates two important changes. Firstly, it removes problems associated with patients losing or not being able to locate the correct script, as their digital script list will always be current in real-time. This reduces the administrative load of re-issuing and re-sending scripts and repeats. Secondly, a combined digital script list makes it significantly easier for clinicians and pharmacies to support patients who have chronic health issues.
The successful rollout of Electronic Prescribing during the pandemic can be largely attributed to the twelve plus years of safe and secure electronic prescription transfer through eRx Script Exchange. eRx functionality, prior to the advent of electronic prescriptions, operated as a parallel electronic process to doctors’ paper-prescribing. eRx helps to ensure prescriptions are dispensed as the prescriber intended, reducing the possibility of misinterpretation or accidental dispensing errors. With more than 31,000 doctors and 5,500 pharmacies using eRx to handle 90% of prescriptions, the system has provided a proven and secure pathway to electronic prescriptions.
In the twelve years since, the prescription exchange service has become the backbone for a range of clinical tools that provide visibility of a patient’s current medication and treatment. Real-time prescription monitoring of Schedule 8 drugs is an example. This displays an alert if a patient’s interactions are at risk of causing an adverse event. According to the Victorian Coroners Court, Victoria’s real-time prescription monitoring, SafeScript, has contributed to reversing a 10-year trend of increasing prescription medicine overdose deaths (showing a reduction for the first time in 10 years, from 405 deaths in 2019 compared to 424 deaths in 2018).
Whilst more attention needs to be given to the follow up mechanisms that support patients once a red flag is identified, real-time interaction flags are a vital clinical tool to help protect patients with dependencies on monitored drugs – and the devastating toll that this takes on their families and communities.
Best Practice Software CEO, Dr Frank Pyefinch, has been an advocate of ePrescribing and sent the very first electronic prescription from our Bp Premier software back in 2009. “Electronic prescribing has come a long way since its early conception back in 2009, which initially focused on the reduction of medication errors from the manual entering of prescription data by pharmacists into their dispensing software. Now clinicians can send prescription data to their patients without the need for paper, making things like telehealth consultations and the good old, ‘I lost my prescription,’ workflows more efficient and safer for both practices and patients.”
“The introduction of other initiatives like real time prescription monitoring (RTPM), under the electronic prescribing umbrella, have introduced additional important clinical safety measures and provided clinicians with important medication data at the point of care. We continue to see great innovation in this space, with plenty more planned changes on the horizon.”
Connecting to a prescription exchange service is fundamental to increasing the visibility of patient medication information, which increases your control over medications. Connecting all of your clinicians to a prescription exchange service is the start.
Co-authored by:
Dr Frank Pyefinch
CEO at Best Practice Software
&
Paul Naismith
CEO at Fred IT
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars