After you upgrade to Topaz Service Pack 1 and begin submitting claims under the Medicare Web Services framework, you will notice different statuses in return messages and the Transactions history, particularly PENDABLE and PENDED.
The new PENDABLE to PENDED workflow may change the way your practice searches for and actions unpaid claims. Best Practice Software recommend actioning PENDABLE claims and resubmitting the invoice immediately if an invoice is returned with PENDABLE, rather than reviewing such claims as an end of day activity.
This article explains why.
For more information on how to resubmit a PENDABLE invoice, review Modify a pendable claim.
What Do the Pending Statuses Mean?
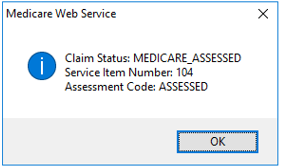
Simple claims that have the Assessment Code of : Assessed do not require manual operator assessment. Such claims are submitted, assessed, and paid or unpaid like they were in previous versions of Bp VIP.net.
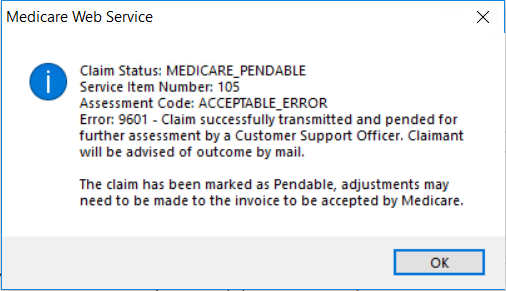
However, if the claim has supporting information such as service text, the claim may require an operator to check the supplementary information provided with the invoice before the claim can be accepted. If this is the case, the claim will return the status of PENDABLE (or MEDICARE_PENDABLE) indicating a further action and resubmission is required.
The PENDABLE status could be applied for several reasons, such as:
- Service text is required for a standard item number, for example, ‘Not normal aftercare’
- Item numbers and duplicate items that require additional service text information, such as reasons for Multiple procedure overrides
- An individual item deemed assessable prior to approval, for example, some diagnostic imaging and pathology items.
Any supplemental information with the potential to require manual assessment can return as PENDABLE, even for otherwise non-complex invoices for item numbers your practice processes daily.
Can I Modify a PENDABLE Claim?
Yes. While a claim is PENDABLE, it has not yet been received for manual assessment by Medicare. This enables you to check that all necessary information is provided in the service text and to immediately resubmit the claim.
Resubmitting the claim to Medicare will update the status to PENDED to notify you that the claim has been received and will be manually assessed by an operator before payment of the rebate to the patient, or notification to the patient of the decline.
While the claim has the status of PENDABLE, two actions can be performed:
- Modify the invoice within the hour of creation to provide more information in the Service Text section under the chevron (F5), and resubmit.
- Reverse or Requote the Invoice if you have made a genuine error and do not wish to proceed with the claim.
How Do I Review and Modify a PENDABLE Claim?
When the claim is in PENDABLE status, you can review and modify the invoice through the patient’s Transactions (F8) screen. Record supplementary information on affected items by clicking on the chevron (>) at the end of line, selecting the appropriate options, and recording service text.
IMPORTANT Once a claim has the status of PENDABLE, you cannot delete either the Payment or Invoice line in Transactions (F8). Reversing or Requoting the Invoice line is the only way of removing the invoices as a Debit.
After you are satisfied with the information provided in the invoice, click the Medicare button on either the Consultation screen or the top of the Transactions screen to send to Medicare and update the claim status to PENDED.
The Lodgement Advice should be immediately printed for the Patient as this is a manually assessed – you may wish to record on the printout the Manual Assessment status to notify the patient. The Lodgement Advice can only be printed when the claim is PENDED, because the claim has been now fully transmitted to Medicare.
Best Practice Software recommend that the Bp VIP.net user immediately actions a PENDABLE claim and resubmits to PENDED so that you are confident the claim has been submitted to Medicare and the Lodgement advice can be printed.
How Long Do I Have to Review a PENDABLE Claim?
The PENDABLE status is only applied to an invoice after the Send Claim button is clicked on the Patient Claims screen for the first time. You have within the hour of invoice submission to review and resend the claim to Medicare (either from the Consultation screen again or from the Transactions F8 screen).
After one hour you will have to repeat the Penable to Pended submission from the Transactions screens to modify and resubmit the claim.
IMPORTANT Because it is essential to resubmit a PENDABLE invoice to PENDED within the hour, Best Practice Software recommend all pendable invoices are actioned immediately.
When Can I Print the Lodgement Advice for the Patient?
You can only print the Medicare Lodgement Advice form when a claim is transmitted with a PENDED status. No Lodgement Advice or Benefit of Claim statement is printed for pendable claims (the claim has not yet been fully transmitted or assessed by Medicare).
Because you receipted the entire balance of the invoice at the end of the consult, Medicare will make payment of the rebate directly to the patient like a normal claim, based on their assessment. Print and give the patient the Lodgement Advice for the claimant’s own record. Your practice may retain a copy in electronic or hard copy form.
Your practice will not receive assessment advice back from Medicare on a Pended claim as this is communicated to the patient or claimant and it is their responsibility to speak to Medicare if their claim is rejected.
For more information on the Lodgement Advice and Benefit of Claim documents, review Medicare Claim Forms.
Can I Same Day Delete PENDED and PENDABLE Claims?
No. Pendable claims have not been fully submitted to Medicare, so won’t show in the same day delete screen.
Pended indicates that the invoice has been resubmitted, so won’t show in the same day delete screen. All deletions must be done by phoning Medicare to action a deletion.
Can I Modify a PENDED Invoice?
You cannot modify a PENDED invoice and resubmit, as the invoice has now been transmitted to Medicare for assessment.
You will need to contact Medicare directly if there are any issues with a MEDICARE_PENDED status claim.
How Do I Find Pendable Claims in the Transactions Screen?
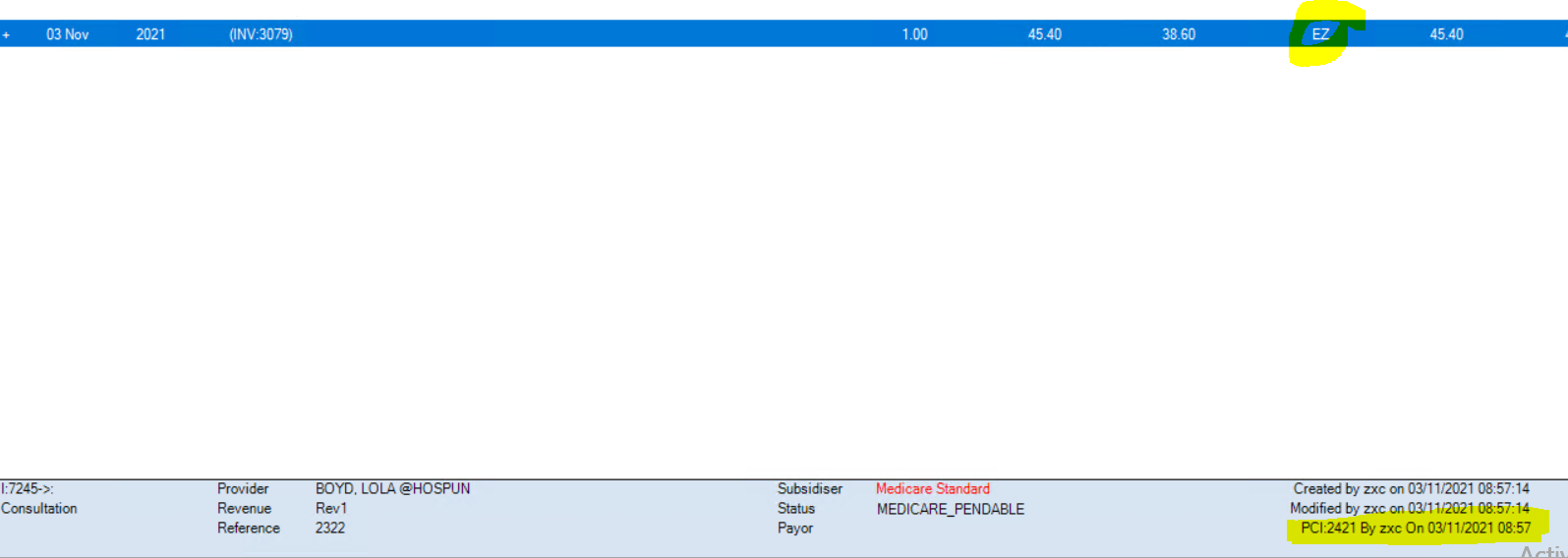
Pendable claims have EZ in the Batch column of the Transactions screen (F8). The Status field in the footer of the Transactions screen also shows the current status of a claim, if the related invoice line in the history is selected.
A pended claim will display with an E for electronic submission and display PENDED in the Status field in the footer of the Transaction screen.
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars