Healthcare consumerism is a concept that has existed for some time, but only recently has it really taken hold and started to significantly impact primary care.
There is perhaps no common understanding as to what constitutes healthcare consumerism, and discussions with providers and patients will likely yield two different sets of responses as to what it actually means.
Ask any provider that has had to contend with correcting the misconceptions of a patient’s self-diagnosis and treatment plan (often courtesy of Dr Google, WebMD or the Mayo Clinic) within the constraints of a few-minutes long consult, and you may be confronted by a somewhat less than flattering take on the subject.
However, as a patient, notions of patient empowerment through clinics and a shift towards patient centricity will likely feature very favourably.
Regardless of your individual view on this, in a consumer-centric society, consumerism was always going to find its way into the healthcare sector, and this will influence the sector in many predictable, but also some unexpected ways. The rate of this change has been accelerating as a result of the general societal changes brought about by COVID-19.
Broadly, consumerism itself has many defining features, but fundamental to it is the principle that the consumer is in control (though subject to marketing, social engineering influences and manipulation). They are in control of what they consume, and their patterns of consumption drive the choices that providers of products and services make about what gets produced and how it is produced. In theory, the more informed consumers are, the more their decisions are driven by knowledge.
It is, then, reasonable to conclude that patterns of consumer behaviour and expectations are responsible for the kind of product and service innovations that organisations like Amazon, Uber and Apple have brought about in their respective industries.
Given the level of disruption that has been brought about by the aformentioned powerhouses in their respective industries, one can only speculate about how much of an impact they would have if they turned their attention to serving the needs of the patient in an era of healthcare consumerism. Even if they don’t – they, and others like them have reset long-held, more traditional consumer expectations.
To compete in this environment, and to compete with the concept of healthcare consumerism itself, provider organisations will have to re-assess their entire value streams, and re-image how to leverage their people, processes and technologies in response to this consumer-centric landscape.
To develop an approach and response, one has to consider some of the behavioural changes brought about by this trend. It does, in essence, come down to the fact that patients’ expectations of care delivery have changed, and that they are taking an increasingly active role through a range of actions.
Patients are, of course, not a homogenous group, so their expectations and their responses to this will differ from one group to another. According to the Pew Research Centre, millennials now make up a larger portion of the population than baby boomers, and the long-term transformations of healthcare will be driven primarily by their needs. This generation has grown up in a technology-rich, consumer focused environment where transparency, rapid delivery and convenience is the norm.
A recent study into healthcare consumer expectations resulted in some startling findings:
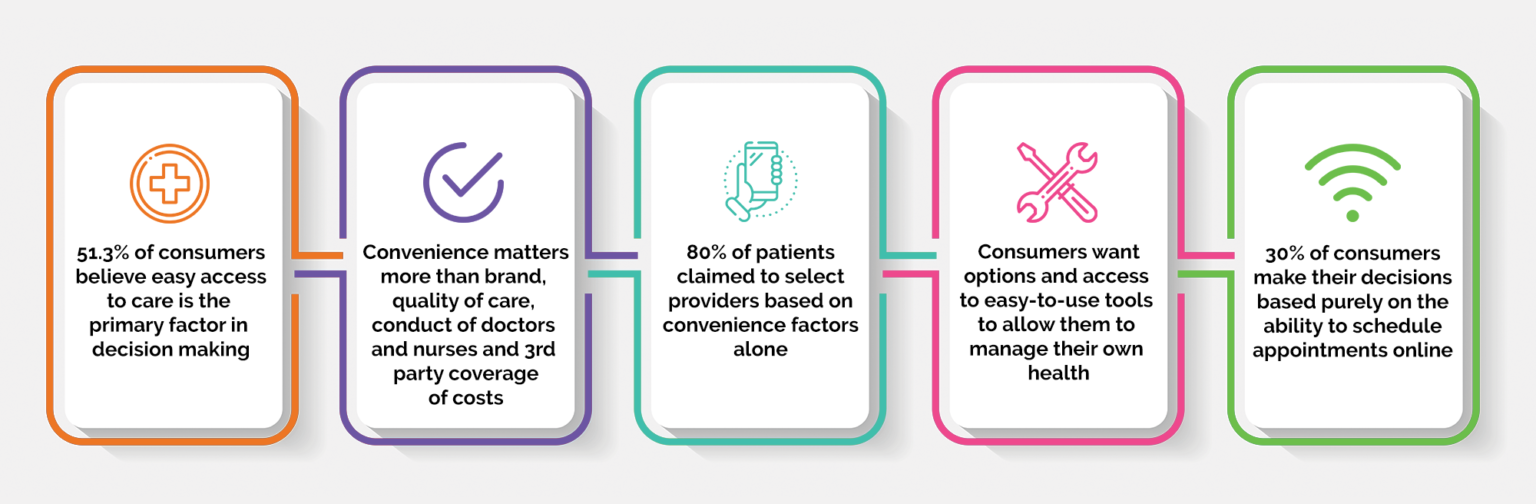
As evidenced by the rise in social media, consumers have proven to be willing to share increasing levels of personal information for the sake of convenience across platforms – as a trend in consumer behaviour, this will likely apply in the context of healthcare as well.
It would be reasonable to expect that patients will want to share information between providers (evidencing a willingness to share), will want to have tools to aid this sharing of information (evidencing the importance placed on convenience), but will in all likelihood require more sophisticated consent and sharing models than what is the norm with some non-health related personal data.
Some of the other actions that patients are taking to meet their expectations include:
- Shopping around, evaluating their options and generally expecting more from providers
- Doing their own research about health issues, treatment options and providers
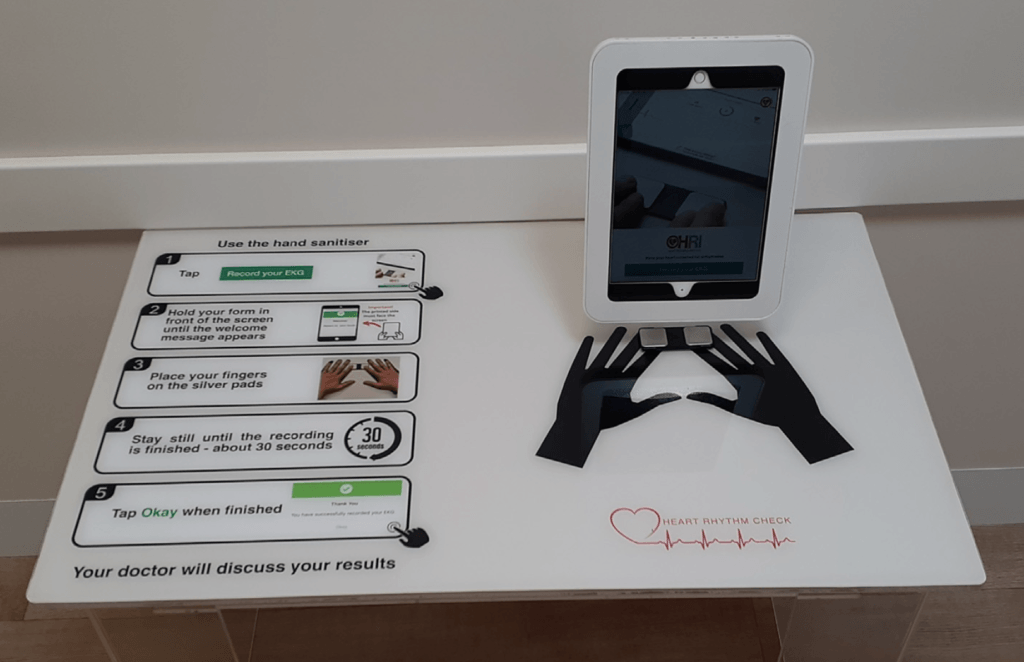
- Taking deliberate steps to monitor and improve their health. The proliferation and increasing sophistication of wearable and home monitoring devices bears witness to this
- Co-operating with providers to make treatment decisions and more freely sharing information with care providers
- Taking cost and quality aspects into consideration in their decision making
- Using technology for appointments, telehealth consults, online payments, prescription renewals and a host of other services
If we consider the expectations and consider the actions patients are taking to meet their expectations, a few things immediately become clear:
- Patient loyalty will continue to decrease as millennials make up an increasing percentage of healthcare consumers
- Providers will face new challenges in attracting and retaining patients, with less loyal patients being more likely to switch providers, and being enabled to do so with the ease provided by technology
- This will have ramifications for health outcomes given the impact on continuity of care
So what’s the message in all of this?
The most logical outcome is that due to the rise of healthcare consumerism, it’s in the industry’s best interest to meet the demands of healthcare consumers by designing products and services that meet current and emerging patient needs.
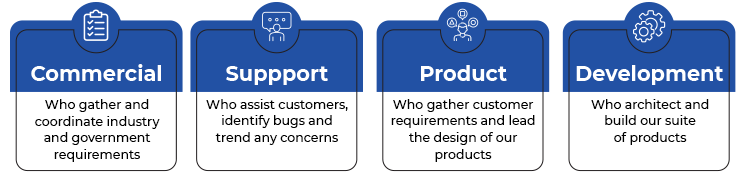
Here at Best Practice Software, we are developing the next generation of healthcare systems that will not only meet the demands of our provider customers, but software that will deliver the tools and meaningful interactions with patients and other stakeholders to address the needs of future healthcare consumers.
Authored by:
Andre Broodryk
Product Manager at Best Practice Software
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars