These days, attracting new patients and retaining existing patients requires an impactful online presence. Looking awesome online will work wonders towards building a recognisable brand and reputation for your practice.
In the increasingly competitive healthcare industry, simply having a website is not enough – you need to be dotted across the internet to appear where your patients are searching. Patients now expect medical practices to have an online presence for sharing information, scheduling appointments, managing reviews, and interacting with patients. Here are 5 simple ways your practice can boost their online presence.

1. Put Your Practice on the Map with a Listing on Google My Business
You could have the best practice in the world, with no wait times and a free lollipop with every visit, but nobody would know if they couldn’t find you! Visibility is important.
Patients usually search for health professionals in their geographic area, so linking your practice to Google Maps is vital. This ensures that your practice’s name and location appear on the map when someone searches your city and “doctor” (or whatever your specialty might be).
There’s no denying that Google reigns supreme in digital marketing. Google My Business is a practice’s one-stop shop for directory listing optimisation. Subscribers’ business information appears on Search, Maps, Google+, and Google Places.
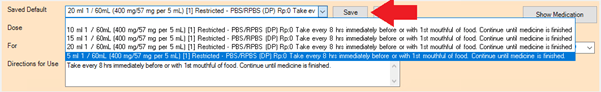
And the best part is it’s free! Create a profile with Google My Business to claim your Google Maps listing. After logging in, you can edit your listing’s contact details, opening hours, photos, and description. You will also be able to see reviews that patients post about your practice and respond to them.

2. Never Underestimate the Power of Social Media
Many
practices think they only need to post professional, business-relevant content. Realistically, fun content, relatable memes or photos of practice staff will
more likely earn you organic and community-focused engagement.
Aim to regularly post content that people want to ‘like’ or ‘share.’ Each interaction will expose your post to new potential patients. Remember, you’re trying to connect with patients, so your content needs to appeal to people outside the medical profession.
Information on social media can directly influence a prospective patient’s decision to choose your practice or even a specific doctor.
Activity on your social media pages can influence where your site appears in Google searches. While the exact SEO impact of social activity is difficult to pin down, there are specific ways to increase your online presence through clever social media usage.
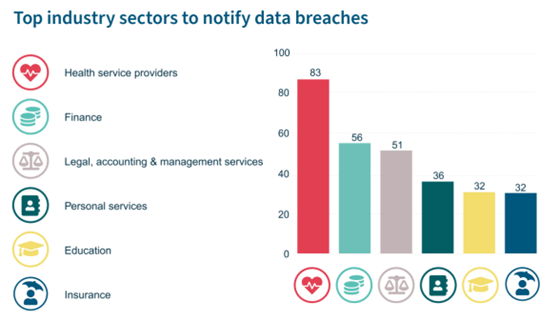
3. Doctor Review Websites = Reputation Management
Many people will search for patient reviews before choosing a new healthcare provider. Online reputation can make or break new patient acquisition. The effort you put into acquiring and managing reviews can lead to acquiring and retaining more patients as well as bringing overall business growth to your healthcare practice.
Online reviews help prospective patients understand the provider’s level of patient care, helping them determine which doctors they should select for their healthcare needs. Practices with a solid online reputation can also help curb a patient’s anxiety, providing reassurance that they are to be trusted with their care.
Encouraging patients to leave reviews is essential for boosting your online reputation. Since unhappy patients may be more likely to share their negative experiences while happy patients continue with their days, the simple act of asking patients for a review can help your practice acquire more positive online reviews.
You might discover your practice already exists on online directories, and people may already be talking about you. Doing a search online will help you find these listings and claim them so you can track what’s happening on them, respond to customer queries, and make any necessary updates. This also applies to some social networks such as Facebook, Yelp, and Google My Business, that allow users to create business listings.

4. Get Into Blogging
Another great way to improve your online presence is to create a blog. Publishing blog posts regularly is a great way to improve your search engine ranking. It also sets you apart by showing off your expertise, which increases your patients’ trust in your service. An engaging blog can also help establish yourself as an industry leader.
When thinking about what to post, focus on content relevant to your audience and related to your area of expertise. You can add value to your content by targeting high-traffic keywords and building links from high-authority websites and credible bloggers. Another way to drive traffic to your blog is by promoting your blog posts on your social channels.

5. Your Practice Website
And finally, the big one – your practice website!
Having a website for your medical practice serves more than one purpose. It is the most concrete and customisable version of your online presence and can supplement how you care for your patients. Your website can be set up to highlight your teams’ areas of expertise and niches, provide patient resources, and streamline the scheduling of patient appointments.
Can your patients book an appointment at 10pm when they feel a sore throat developing? Including an online booking widget on your website will allow you the capture appointment bookings long after your reception staff have signed off for the evening.
Building a practice website can seem like a big task, but it is well worth it in the long run. You can hire a professional to create your website or do it yourself.
Whether the patient has recently moved to a new area or is switching practices for other reasons, people will naturally look online to see their options. If your practice does not have a website, you may be missing out on a precious opportunity to attract new patients.
Authored by:

Lucy Saul
Marketing & Communications Specialist at Best Practice Software
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars