Working on improving workplace communication is paramount for any business, and Medical Practices are no exception.
As a Practice leader, you know that success in your role is dependent on your ability to effectively communicate. But just as important as the quality and value of your own words is the cultural commitment you make to internal communication within your Practice as a busy, high-profile workplace. So how do you make it part of everyday business, and embed it within Practice business strategy to make it “part of what we do around here”?
I recommend promoting the benefits of good workplace communication within your team by outwardly recognising that good communication is fundamental to the success of your Practice as a business. By making communication one of your ‘people pillars’, you’ll ensure less misunderstanding within your team – including Practitioners, Reception, Practice Management, and IT/business support team –, an increased commitment to change, a reinforced role of supervisor as leader, and more active participation in the Practice and its mission.
Think about adopting some shared communication principles within your Practice team, like:
- Embedding in your team mission your commitment to open, honest, and meaningful internal communication – at all costs, including the potential to damage fragile egos. Embrace the concept that, as leader, you’ll set the highest standard in being transparent and authentic in your communication with the team and invite members to (respectfully) challenge you anytime they think you miss the mark.
- Embrace face-to-face communication foremost while still recognising e-mail and intranet bulletins as a convenient, but ultimately more impersonal, workplace tool. Sunrise (before clinic) and Sunset (after clinic) personal team or individual briefings will always be more valued when they’re localised, purpose-driven, two-way, … and brief.
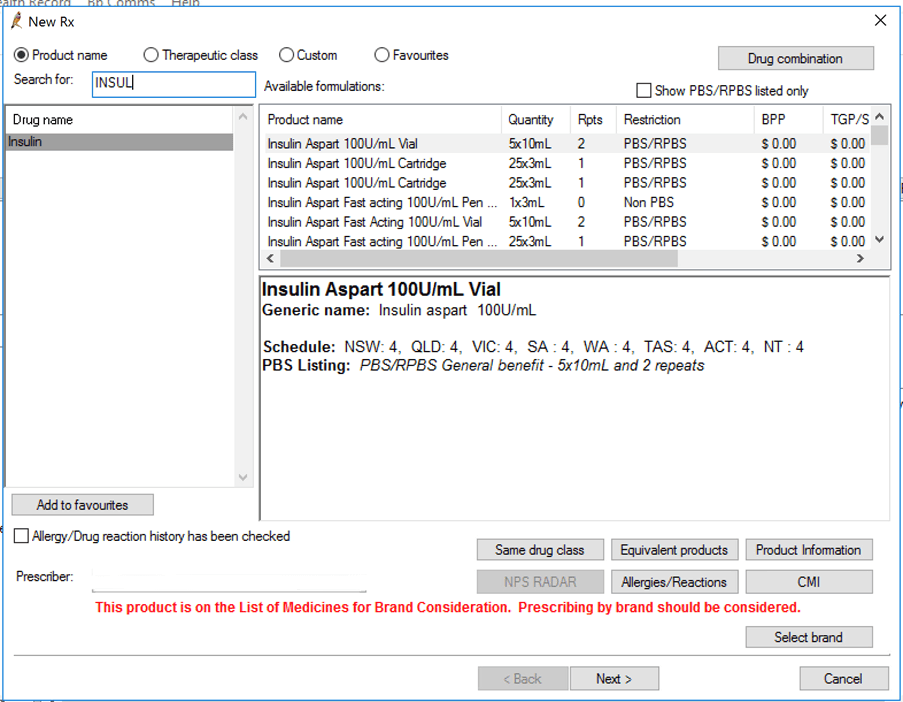
- Utilise the communication tools already built into your business software/systems for instant messaging when you need to raise attention to an urgent or immediate matter – especially between Practitioner and Reception team. There is a great internal messaging feature built in to Bp Premier that many doctors and their Practice team use, providing a useful instant on-screen message if ever required.
- Value meaningful two-way engagement with your Practice team, ensuring the team knows you will provide (and you welcome back) genuine and constructive feedback on team achievement towards individual and shared goals. Improving workplace communication is a lot easier when your team knows they’re being listened to.
- Recognise the frontline role your Practitioners and Practice leadership team plays in team engagement – and let your Practice leaders know you expect they will make team communication the first and foremost part of their role as leader and use language which is familiar to and understood by their work group.
- Ensure your Practice team knows they will be briefed face-to-face on matters which affect their job, and you’ll set that standard yourself. If each employee can’t be consulted and involved in decision-making regarding their job before any major change occurs, they should at least be briefed in person on important matters which change what they do, or how you expect them to do it.
- Preference communication that promotes action within your team and Practice. We’ve all sat in a meeting that should have been an email, so ensure any team assemblies have a clear and concise purpose (agenda), don’t linger longer than is necessary, and you note and distribute a summary of key action items and accountabilities before anybody leaves.
- Outline to the team your minimum engagement opportunities. Perhaps make a commitment that, for instance, you’ll host supervisor briefings at least monthly, and supervisor-to-Practice team briefings every second day, and informal ‘toolbox’ chats on health and safety matters or reception/patient matters each Friday morning at 7:30am. This helps ‘lock in’ your time together, and shows you’re wholly committed to these engagements, even if you don’t have much news to share.
While these tips provide a good starting point on the topic, improving workplace communication needs and deserves follow through and actions that match your words, from the senior-most level to the people greeting and treating your patients. By sharing team news early and consistently you’ll help ensure your preferred (rather than speculative) message is heard by every member of your team.
Authored by:
Craig Hodges
Chief Corporate Officer at Best Practice Software
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars