With face-to-face patient contact being limited due to quarantine, lockdowns, and illness, phone consults are now the new normal. Telehealth notes are recorded as part of a consultation, but what about recording other phone calls or communication with patients? This is where Bp Premier Contact Notes can assist, and in this article I’ll offer some tips on how to use them. If you haven’t utilised them before, let’s take a minute to introduce how they can be of benefit to you and your Practice.
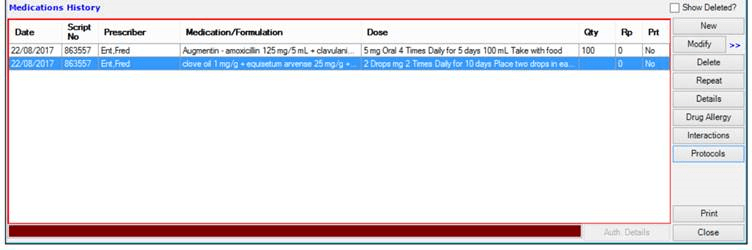
A Contact Note represents any attempt by the Practice to contact a patient by phone, letter, SMS, mobile app, or even when using external email applications. It will record the essentials: when contact was made, who the contact was with, what the contact was about, how the contact was made, and the success status.
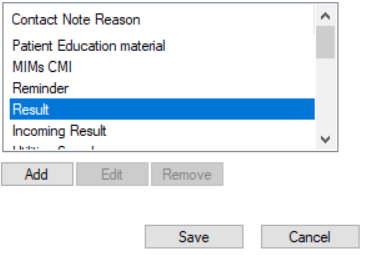
One of the great things about Bp Premier Contact Notes is that your Practice can create customised contact reasons specific to your team, like chasing up overdue invoices, speaking with a specialist on behalf of patients, or booking an ambulance transfer.
You can add new reasons quickly and easily by accessing Setup > Configuration > Lists tab
- Click Add under the list. The Reason for contact note window will appear.
- Enter your new contact reason: Specialist bookings.
- Click Save.
- Click Save again and close the Configuration screen.
Contact Notes are designed to not only support your patients, but also to support your team and business practices.
More Contact Note Tips in Bp Premier are available on our Knowledge Base from within Bp Premier. Click on Help > Online and search ‘Contact Notes’.
Authored by:
Belinda Bazant
Content Developer at Best Practice Software
Explore our range of news and training resources:
Bp Learning Video Library | Bp Learning Training Options | Bp Newsroom Blog
Subscribe to Our Newsletters | Bp Learning Webinars